- LOGIN
- MemberShip
- 2025-12-22 09:42:33
- Company
- Multinational pharma's ave. salaries amount to KRW 100m
- by Son, Hyung Min Apr 22, 2025 05:59am
- Last year, the average annual salary for employees at the Korean subsidiaries of major multinational pharmaceutical companies surpassed KRW 100 million, with Sanofi‑Aventis Korea and Gilead Sciences Korea close to KRW 150 million. According to an analysis of the 2023 audit reports filed by 30 foreign pharma subsidiaries on the Financial Supervisory Service (FSS)’s web board on April 21, the average basic salary per employee amounted to KRW 105.2 million, and 18 of those companies reported average pay above KRW 100 million. The average salary per individual reflect only base salaries as disclosed in the audit reports, excluding fringe benefits, bonuses, performance incentives, and retirement payments are excluded, so actual take‑home pay may differ slightly. 2023 Annual Salaries for Employees at the Korean Subsidiaries of Major Multinational Pharmaceutical Companies Sanofi‑Aventis Korea ranked the highest, with an average annual salary of KRW 147.31 million. Last year, its total salary expense rose 61.8% to KRW 53.62 billion from KRW 33.13 billion in 2022, even though its headcount fell by six to 370 employees. Performance‑related pay also climbed markedly, with the company disbursing KRW 3.29 billion in incentives, up 30.9% from the prior year. Gilead Sciences Korea ranked second, with its average per individual salary rising from KRW 128.60 million in 2023 to KRW 141.32 million last year. Its total payroll expense increased by 14.5%, from KRW 11.61 billion in 2023 to KRW 13.28 billion. Boehringer Ingelheim Korea also saw substantial growth in compensation. With headcount unchanged at 164 employees, its average salary climbed by 9.4% to KRW 139.80 million, and total salary outlays rose by KRW 775.35 million. Pfizer Korea’s average salary jumped to KRW 126.24 million, up roughly KRW 25 million from KRW 99.95 million the year before. The primary driver was a global early‑retirement program (ERP). Pfizer implemented a global restructuring initiative throughout 2023 and into last year in response to a sharp decline in vaccine and therapeutic revenues following the transition to endemic COVID‑19. This strategic decision also led to workforce reductions at its Korean subsidiary. Pfizer Korea's ERP led to a headcount reduction from 454 in 2023 to 404 last year; severance pay paid under that program totaled KRW 5.335 billion, a 279.9% increase over 2023. At Kyowa Kirin Korea, severance costs outstripped total salaries. While the company paid out KRW 8 billion in salaries, it recorded KRW 26 billion in retirement benefits. Kyowa Kirin implemented ERP last year. Kyowa Kirin's Asia‑Pacific restructuring last year included selling its China unit to Hong Kong’s Winhealth Pharma Group and transferring domestic and key Asia promotional and distribution operations to DKSH. Kyowa Kirin sells a portfolio of novel therapies, such as the erythropoiesis‑stimulating agent 'Regpara,' anemia treatment 'Nesp,' and neutropenia therapy 'Neulasta,' and reported stable sales of KRW 92.4 billion in 2022 and KRW 98.3 billion last year. The company says it has restructured to focus on its new pipeline in antibody and cell & gene therapies. Other multinational subsidiaries paying average salaries above KRW 100 million include Viatris Korea, Ipsen Korea, UCB Korea, GSK, Janssen Korea, Ferring Korea, AbbVie Korea, BMS Korea, LundBeck Korea, Abbott Korea, Galderma Korea, and AstraZeneca Korea. Some firms may have higher take‑home pay than reported salary. For example, MSD Korea, which reported an average salary of KRW 67.7 million, logs portions of its R&D and other staff compensation under operational research and development expenses or cost of goods sold rather than base payroll. Otsuka Korea reported KRW 24.7 billion in selling and administrative payroll expenses, contrasting with KRW 47.0 billion. The company recognizes some units' salaries as employee‑related costs because certain departmental salaries are classified under production or R&D.
- Policy
- MFDS turns down Jeffty’s integrated Phase II/III trial
- by Lee, Hye-Kyung Apr 22, 2025 05:59am
- The Ministry of Food and Drug Safety has rejected the clinical trial protocol for Hyundai Bioscience's COVID-19 drug Jeffty that the company submitted last year. According to the minutes of the MFDS's Central Pharmaceutical Affairs Council meeting that was released on the 17th, the council agreed that the integrated Phase II/III clinical trial protocol submitted by Hyundai Bioscience was not valid and that a separate Phase II clinical trial was necessary. Hyundai Bioscience plans to respect the regulating authority's judgment and comprehensively review the regulatory standards, scientific evidence, and global strategy within 60 days of the appeal period and prepare a response. During the COVID-19 pandemic, Hyundai Bio conducted a Phase II dose-finding clinical trial for emergency approval of Jeffty. At the time, the company submitted a clinical trial plan for 300 patients for two dose groups of Jeffty 0 300mg and 450mg - and completed the clinical trial with the participation of 11 institutions and the consensus approval of the Data & Safety Monitoring Committee. Based on the results, Hyundai Bioscience submitted an integrated Phase II/III clinical trial protocol for the 300 mg monotherapy dose last year. In this regard, a CPAC member pointed out that “the design proposed by the applicant is Phase II/III trial, but the trials are not connected. The Phase II and III trials are separate. Even if the applicant tries to quickly approach approval with a Phase II/III design, it is not a COVID-19 emergency situation anymore, and the drug itself does not seem to have a basis for urgent use.” Most CPAC members felt that it would be appropriate to conduct a separate Phase II trial, rather than a Phase II/III trial and reapply for a Phase III trial after confirming its effect. “Phase II/III designs have the advantage of saving time and money over traditional designs, but they also have disadvantages,” said one committee member. Phase II/III trials are not used for vaccines or therapeutics, but it has been used for anticancer drugs. The MFDS explained that “Phase II/III trial is limited to cases where anticancer drugs are rare and difficult to recruit patients or require a long period of time to evaluate. The Phase II/III design used in such cases is different from the plan set for Jeffty, which is a Phase II/III design that validates the drug’s efficacy mid-trial and discontinues the trial if it is not effective.” In the case of Jeffty, it was suggested that a Phase IIa dose-finding trial should be conducted first, as the existing Phase II trial did not confirm efficacy or adequately explore the dose. “A Phase IIa trial should at least explore the dose in order to determine the feasibility of advancing to the next stage, but the current application design is not appropriate in the absence of dose exploration,” said one member. Therefore, the CPAC unanimously concluded that a Phase II trial should be conducted independently for Jeffty first, and a justification for the dose setting should be provided. “This administrative procedure is not an evaluation of the efficacy or safety of the treatment, but a request for adjustments to the clinical approach,” said Hyundai Bioscience. “We will prepare a strategy that is in line with global standards.”
- Policy
- Boryung's follow-on drug referencing 'Lenvima' to be reimb
- by Lee, Tak-Sun Apr 22, 2025 05:59am
- Product photo of LenvimaThe first follow-on medicines developed by Boryung similar to Lenvima (lenvatinib mesylate) is expected to be added to the reimbursement listing in May. This drug is made by addition of the new dimethyl sulfoxide (DMSO) solvate to the original Lenvima. The drug's supporting document has been submitted and it was approved by the Ministry of Food and Drug Safety (MFDS) in February. The original Lenvima's patent has been expired, but the follow-on patents, including usage patent, are still effective. Lenvima's company is still fighting Boryung regarding this, so future responses from two companies are gaining attention. According to industry sources on April 21, Lenvanib Cap 4 mg (lenvatinib mesylate dimethyl sulfoxide) This drug references Eisai's Lenvima Cap 4 mg (lenvatinib mesylate). Lenvima Cap 4 mg is reimbursed for KRW 29,739. Lenvanib Cap 4 mg was priced at 90% of the original drug because pharmaceuticals that submit supporting documents and are developed by changing salt or as isomer are priced at 90% of the ceiling cap of the targeted product. The MFDS concluded that adding new solvate (dimethyl sulfoxide) can be categorized into new salt, so it approved Lenvanib Cap 4 mg as a pharmaceutical with an active ingredient containing new salt. At the time of obtaining MFDS approval in February, Boryung was approved for Lenvanib Cap 4 mg, Lenvanib Cap 10 mg, and Lenvanib Cap 12 mg. Among these, 12 mg is not available for the original drug. However, only the 4 mg product will likely be added to the reimbursement list in May. The rest of the products will be considered for the reimbursement process later. Lenvanib Cap 4 mg's addition to the reimbursement list was possible because the original product's substance patent expired on the 4th of last month. Boryung continues to challenge other follow-on patents, including usage patent, through patent trials. The final patent dispute outcome is expected to impact Lenvanib sales. The approval indication for Lenvanib Cap 4mg is the same as that of the original Lenvima Cap 4 mg. Both drugs are approved for multiple indications, including 1. the treatment of radioiodine‑refractory, locally recurrent or metastatic progressive differentiated thyroid cancer; 2. first‑line therapy for unresectable hepatocellular carcinoma; 3. in combination with pembrolizumab in patients with advanced endometrial cancer, without the conditions of MSI-H (microsatellite instability-high) or dMMR (mismatch repair deficient) mismatch repair–proficient, who have progressed on prior systemic therapy and are ineligible for surgery or radiotherapy; 4. first‑line treatment of advanced renal cell carcinoma. A legal dispute between the companies is anticipated because number 3 and 4 indications are related to usage patents. Lenvatinib mesylate is a tyrosine kinase inhibitor that blocks vascular endothelial growth factor (VEGF) and fibroblast growth factor (FGF) receptors to suppress angiogenesis and tumor proliferation. It is currently reimbursed for the treatment of hepatocellular carcinoma and differentiated thyroid cancer. The original Lenvima's sales in 2023 amount to KRW 10.3 billion, based on IQVIA.
- Company
- Darzalex SC may be prescribed at general hospitals in KOR
- by Eo, Yun-Ho Apr 22, 2025 05:59am
- The subcutaneous injection formulation of the multiple myeloma drug Darzalex may now be prescribed at general hospitals in Korea. According to industry sources, Janssen Korea's Darzalex SC (daratumumab) has passed the drug committees (DCs) of tertiary hospitals in Korea, such as the Seoul National University Hospital and Seoul Asan Medical Center. Darzalex SC dramatically reduces administration time and infusion-related reactions compared to existing intravenous drugs and is approved for a total of 6 indications and five regimens. It was approved in Korea in 2020. The SC formulation was approved for a total of 6 indications and 5 regimens, including “combination therapy with bortezomib, melphalan, and prednisone (DVMP) for newly diagnosed multiple myeloma patients who are not candidates for autologous stem cell transplant” and “combination therapy with bortezomib, thalidomide, and dexamethasone (DVTd) for newly diagnosed multiple myeloma patients who are candidates for autologous stem cell transplant,” and “combination therapy with lenalidomide and dexamethasone (DRd) for newly diagnosed multiple myeloma patients who are not candidates for autologous stem cell transplants.”. Also, the drug can be used by “patients with relapsed or refractory multiple myeloma who have received at least one prior therapy lenalidomide in combination with dexamethasone (DRd) for;” “patients with multiple myeloma who have received at least one prior therapy with bortezomib and dexamethasone (DVd)” and “patients with refractory multiple myeloma as monotherapy after they have failed at least 3 prior therapies, including each of a proteasome inhibitor and an immunomodulatory agent.” Among the indications, the drug’s reimbursement coverage was extended in February to cover its use as first-line therapy as part of a four-drug combination therapy (DVTd therapy) that includes Darzalex in patients with multiple myeloma who are eligible for autologous stem cell transplant. Darzalex SC is a fixed-dose formulation that can be administered over approximately 3-5 minutes. This is a significant reduction in dosing time compared to the 3.5 to 6.5 hours required for intravenous Darzalex. In addition, the incidence of systemic infusion-related reactions was reduced by two-thirds compared to intravenous Darzalex, which is expected to significantly improve patient convenience and potentially deliver efficiencies in the multiple myeloma treatment setting. Meanwhile, the US-based Halozyme Therapeutics’s human hyaluronidase technology enabled the formulation change of Darzalex. Halozyme and the Korean company Alteogen are companies that are attracting attention globally for their SC formulation change technology. Drug delivery to the subcutaneous tissue has been challenging due to its hyaluronic acid protection. However, the use of “human hyaluronidase” enables the breakdown of hyaluronic acid. The SC formulation change technology enhances the permeability of subcutaneous tissue, allowing the drug to rapidly disperse in the subcutaneous tissue and be absorbed into the bloodstream.
- Company
- Can 'indication-based pricing' become a reality?
- by Moon, sung-ho Apr 22, 2025 05:58am
- With the presence of anti-cancer drugs in the clinical field becoming more prominent in recent years, multinational pharmaceutical companies have been calling for a new reimbursement system. In addition to existing immuno-oncology drugs, the emergence of antibody-drug conjugates (ADCs) has increased the number of treatments that are effective against multiple cancers, and the industry requests different drug prices to be applied for each so-called 'indication.’ In fact, the multinational pharmaceutical industry has been requesting so for the past decade, but it hasn't made much of a difference. However, as obesity drugs have expanded their indications to include diabetes, cardiovascular disease, and metabolic dysfunction-associated steatohepatitis (MASH), the debate is no longer limited to anti-cancer drugs. # According to industry sources on the 21st, immuno-oncology drugs or ADCs with indications for various cancers have recently been introduced into the domestic clinical field, and opinions have been raised that different drug prices should be applied to the same drug for different indications. This method - Indication-based pricing (IBP) - is a further subdivision of value-based pricing (VBP), which states that drug prices should reflect the actual value of drugs. Currently, the single-price policy utilized by Korea’s health insurance system is based on the initial indication. For each additional indication, the existing drug price must be reduced to cover the expanded area of reimbursement. For example, if an A immuno-oncology drug is first approved for lung cancer, and then expands its indications to include gastric and breast cancer, the existing drug price must be reduced through pricing negotiations as its use in practice increases under the current system. In other words, the more you expand reimbursement by adding indications, the more you have to reduce the drug price. The problem is that as the number of therapies with indications for multiple cancers, such as major immuno-oncology drugs and ADCs, grows, so does the demand for their reimbursement, and the current single-price policy cannot accommodate them all. So the more approvals for indications and reimbursement the pharmaceutical companies receive, the more pressure they face to reduce drug prices. As a result, the Korean Research-based Pharmaceutical Industry Association (KRPIA) recently requested the government to launch pilot projects on 'blended pricing' (indication-weighted average price) and 'differentiated reimbursement rates by indication' within the framework of Korea’s risk-sharing agreement (RSA) system. Blended pricing is a system that has been implemented in Italy, France, Japan, and other countries. The idea is to set a single price for a drug, but calculate a weighted average price for each indication based on expected usage and clinical value. The main content is to agree on a single price for the same drug while adding reimbursement in consideration of the increased patient and input of financial resources when the reimbursement standard is extended. The industry request is for the blended pricing system to be introduced first, then the risk-sharing system to be improved by applying differential reimbursement rates by indication. In this regard, Ewha Womans University Professor Jung Hoon Ahn (College of Science& Industry Convergence) recently published a study on 'Reimbursement Policy for Multiple Indication Drugs' sponsored by AstraZeneca. In fact, it reflects the will of the multinational pharmaceutical industry, led by the KRPIA, to introduce the system. “The blended pricing method is highly feasible in the domestic reimbursement and drug pricing environment,” said Professor Ahn. “Blended pricing can be implemented in the legal contract stage, applying it at the risk-sharing agreement scheme stage.” “Blended Pricing can be applied within the risk-sharing framework to reflect the value of drugs per indication while managing the financial risk of drugs with uncertain cost-effectiveness,” he said. ”Combined with a structure that allows for reassessment based on actual usage data or adjustments to reimbursement terms based on indication-specific usage, this can increase policy flexibility and feasibility.” As the multinational pharmaceutical industry has been pushing for the introduction of the program, attention has naturally turned to the government’s acceptance. While the need to introduce the system is well understood, as it has been called for more than a decade, there is also consensus that the agenda is not urgent enough to prioritize and pilot quickly in the course of Korea’s current health insurance system. At the same time, there is also an opinion some companies have been particularly exerting their influence among multinational pharmaceutical companies. There are doubts that the benefits of its institutionalization may be concentrated on certain pharmaceutical companies. This would naturally lead to equity issues with other pharmaceutical companies and the domestic pharmaceutical industry. A law firm advisor who serves as a high-ranking government official gave a sobering assessment, saying, “The multinational pharmaceutical industry has been asking for such a system, but it is doubtful that social consensus can be made on this, regardless of whether the government accepts it or not.” “The key to the indication-based drug pricing system is to accurately predict the usage of each drug,” he said. ”Even now, when discussing expanding the scope of use of a drug, the price is reduced in anticipation of the increased volume. However, when we look at future outcomes, it often doesn't work well,” he said. In other words, it is difficult to introduce blended pricing at a time when even the estimated usage for risk-sharing is not always accurate. It is theoretically possible, but it is difficult to apply it in practice. “If there is a need to introduce the system, the government should prioritize judging its effectiveness through research services,” said HIRA Director Kook-Hee Kim. “No proper monitoring has been made yet. The weighted average should be discussed every time the number of therapeutic indications increases and the impact should be analyzed in various ways,” indicating that it is a long-term challenge.”
- Company
- Zuellig Pharma's performance fluctuates after a brief reboun
- by Son, Hyung Min Apr 21, 2025 05:54am
- Zuellig Pharma Korea, a global pharmaceutical distributor that had experienced ups and downs in its external growth, successfully rebounded last year. Zuellig Pharma's sales declined for 4 consecutive years after recording sales of over KRW 1 trillion in 2020 but showed signs of recovery by taking on the domestic distribution of new drugs from multinational pharmaceutical companies. According to the Financial Supervisory Service on the 18th, Zuellig Pharma's sales last year were KRW 889.3 billion, up 4.8% from the previous year. Operating profit was KRW 4.3 billion, similar to the previous year. Zuellig Pharma is the Korean subsidiary of a Swiss global pharmaceutical distribution company that entered the Korean market in 1998. As the first global distributor to enter the Korean market, it faced strong opposition from the domestic industry. The Korea Pharmaceutical Distribution Association formed the Zuellig Countermeasures Committee and took strong measures to prevent Zuellig Pharma from monopolizing the supply of global pharmaceutical companies' products. Nevertheless, Zuellig Pharma's sales continued to grow until 2021. The company's sales grew steadily from KRW 706.9 billion in 2015 to KRW 889.4 billion in 2016, then to KRW 970.9 billion in 2017. Zuellig Pharma recorded KRW 1.184 trillion in 2019, becoming the third company to exceed KRW 1 trillion in sales after Geo-Yong and Baekje Pharmaceutical. The company maintained its status in the trillion-won club in 2020 with sales of KRW 1.0372 trillion, but sales fell to KRW 910 billion the following year. In 2022, sales amounted to KRW 885.3 billion, a 2.7% decrease from the previous year. In 2023, sales decreased by 4.1% year-on-year to 850 billion won. Zuellig Pharma was hit hard by changes in the drug distribution environment. Before, Zuellig Pharma had grown through exclusive deals with multinational pharmaceutical companies. In particular, domestic drug distributors had to sign wholesale contracts with Zuellig Pharma in order to distribute drugs from multinational pharmaceutical companies. However, major multinational pharmaceutical companies began to utilize the distribution networks of Korean pharmaceutical companies, forging co-promotion agreements with domestic companies, gradually reducing Zuellig Pharma's market share. In addition, domestic pharmaceutical distributors obtained distribution rights through direct contracts with multinational pharmaceutical companies, reducing Zuellig Pharma's main source of revenue. For example, Geo-Yong directly distributes UCB Korea’s allergy treatment Zyrtec, and psoriasis treatment Bimzelx. Geo-Yong is also selling over-the-counter (OTC) drugs from multinational pharmaceutical companies, such as the contraceptive Mercilon. Furthermore, major domestic companies have established new logistics systems such as 3PL and 4PL to enhance their competitiveness. Logistics systems are categorized into four types (1PL/2PL/3PL/4PL) based on their structure. 3PL refers to outsourcing logistics operations to external companies, while 4PL refers to customized services that not only outsource logistics but also provide consulting on suitable logistics systems and IT-related solutions. Larger companies have adopted integrated logistics strategy models, establishing their own logistics IT systems and strengthening order, receivables, and collection management functions. As a result, Zuellig Pharma now faces competition in the utilization of 3PL/4PL logistics systems as well. In particular, domestic companies have equipped themselves with cold chain systems and are distributing major biological products such as Dupixent, putting a brake on Zuellig Pharma's external growth. Operating profit rebounded, but competition intensified In addition to Zuellig Pharma, other global pharmaceutical distribution companies such as DKSH and DB Schenker Korea, as well as domestic firms like Pico Innovation and Bluemtec have established online platforms, intensifying market competition. However, Zuellig Pharma managed to rebound last year with its first sales increase in 4 years. In particular, operating profit has also improved recently. Zuellig Pharma posted operating losses every year from 2017 to 2021. However, in 2022, it returned to profit for the first time in about 7 years with KRW 900 million. In 2023 and last year, it recorded KRW 4.3 billion, showing growth. Zuellig Pharma succeeded in increasing its operating profit by improving its cost ratio along with a reduction in sales and administrative expenses and employee wages. Thanks to its improved performance, Zuellig Pharma emerged from total capital erosion, which had continued for 2 years since 2020. Total capital erosion refers to a state in which a company's deficit grows so large that its surplus runs out and even its paid-in capital is eroded, resulting in negative total capital. Zuellig Pharma was in a state of complete capital erosion in 2020 and 2021, with total capital of – KRW 1.5 billion and -KRW 14.5 billion, respectively. Zuellig Pharma plans to achieve growth in sales and operating profit through the distribution of innovative new drugs. Last year, Zuellig Pharma became responsible for the distribution of the obesity treatment drug Wegovy. Wegovy is a glucagon-like peptide (GLP-1) obesity treatment that recorded sales of over KRW 60 billion in the fourth quarter of last year alone. Zuellig Pharma successfully secured the distribution rights for Wegovy thanks to its experience in distributing the obesity treatment Saxenda. Zuellig Pharma will also be responsible for the domestic distribution of the immuno-oncology drug Libtayo. Libtayo (cemiplimab) is currently approved in South Korea as a first-line monotherapy for advanced non-small cell lung cancer and as a treatment for metastatic or locally advanced cutaneous squamous cell carcinoma (CSCC) and recurrent or metastatic cervical cancer. Last year, Zuellig Pharma also formed a partnership with European consumer healthcare company Karo Healthcare to target the Asian market and signed a domestic distribution agreement for the athlete's foot treatment Lamisil.
- Company
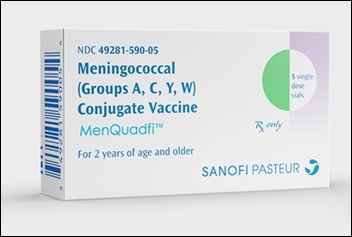
- Sanofi’s MenQuadfi to be launched soon in Korea
- by Whang, byung-woo Apr 21, 2025 05:54am
- Sanofi's next-generation meningococcal vaccine is set to launch just 1 year after receiving approval in Korea, signaling the start of intense market competition. Pic of MenQuadfi According to industry sources, Sanofi is preparing to launch its invasive meningococcal disease vaccine MenQuadfi in the third quarter of this year. MenQuadfi is a fully liquid vial quadrivalent meningococcal vaccine that prevents meningococcal serotypes A, C, W, and Y, and is approved for a single dose for individuals aged 2 to 55 years. When compared for immunogenicity with existing quadrivalent meningococcal vaccines, MenQuadfi demonstrated non-inferiority for all four serotypes. Unlike Sanofi's existing meningococcal vaccine, which utilized the diphtheria toxid protein, MenQuadfi utilizes the tetanus toxoid protein and has increased antigen amount. Currently available meningococcal vaccines include GSK Korea’s Menveo and Sanofi’s Menactra. Both vaccines are indicated for the prevention of invasive meningococcal disease caused by Neisseria meningitidis serogroups A, C, W135, and Y. With the launch of MenQuadfi, the competitive landscape is expected to shift from “Menveo vs. Menactra” to “Menveo vs. MenQuadfi.” Sanofi has decided to discontinue Menactra upon the launch of MenQuadfi, but the exact timing of supply discontinuation will be dependent on market inventory levels. A Sanofi representative stated, “We decided to launch MenQuadfi based on the high demand for Menactra in the global market and the expansion of its indications. As a result, we have decided to discontinue Menactra. We will do our utmost to ensure an uninterrupted supply of meningococcal vaccines in the Korean market by adjusting the launch schedule of MenQuadfi in accordance with the depletion of Menactra inventory.” One of the differences between Menactra and MenQuadfi is the age at which they can be administered. Menactra can be administered from 9 months of age, while MenQuadfi is currently available as a single dose for individuals aged 2 to 55 years. However, as the age range for MenQuadfi is being expanded, the vaccine is expected to naturally replace Menactra in the market. In particular, while Menactra contained 4ug of meningococcal serum antigen, MenQuadfi contains 10ug of all four antigens. Meningococcal vaccination costs, from left, GSK Menveo Sanofi Menactra (Data = HIRA Before MenQuadfi’s launch, GSK had already launched Bexsero, a meningococcal group B absorbed vaccine. Bexsero is a vaccine for preventing meningococcal group B infections and differs from the existing Menveo in its scope of prevention. In other words, GSK has introduced a new meningococcal vaccine with a different scope of prevention, while Sanofi has unveiled a next-generation vaccine with enhanced prevention effects. According to IQVIA data, Menveo's sales in 2023 were KRW 52 billion, while Menactra's sales were KRW 5 billion. Given the significant sales gap between the two products, both companies are expected to focus on increasing their market share with the launch of next-generation vaccines. However, meningococcal vaccines are not classified as essential vaccines and are classified as premium vaccines, so price accessibility is expected to be an important factor. According to the Health Insurance Review and Assessment Service's non-reimbursable medical expenses, Menveo costs an average of KRW 142,805, while Menactra costs an average of KRW 142,072.
- Company
- Roche Korea's 'Lunsumio' available at general hospitals
- by Eo, Yun-Ho Apr 21, 2025 05:54am
- Product photo of Lunsumio The first GIFT-designated drug 'Lunsumio' can now be prescribed in general hospitals. According to industry sources, Roche Korea's CD20xCD3 bi-specifc antibody 'Lunsumio (mosunetuzumab)' has passed the drug committee (DC) of Asan Medical Center in Seoul. Lunsumio is the first medicine to be designated as a 'Global Innovative products on Fast Track (GIFT)' and obtained approval from the Ministry of Food and Drug Safety (MFDS) in November 2023. This drug can be prescribed for adult patients with relapsed or refractory follicular lymphoma (FL) after two or more systemic therapies. However, Lunsumio remains a non-reimbursed drug. Roche has applied for the 'approval-assessment package system,' in addition to the GIFT designation, but discussions on reimbursement have yet to progress. FL is a type of non-Hodgkin Lymphoma (NHL) that occurs when cells in the lymph system turn malignant. Because the symptoms of the disease progress slowly, about 80% of the cases are identified at stage III or Stage IV after the disease progresses. The prognosis for patients who relapse is poor. Median progression-free survival (mPFS) is 10.6 years for patients who received first-line treatment; however, mPFS drops to two years with third-line treatments, representing about 20%. Lunsumio is the first-in-class CD20xCD3 bi-specific antibody involving T cells for relapsed or refractory FL. It simultaneously binds to a protein CD3 on the surface of T cells, which are types of white blood cells and immune cells, and protein CD20 of the malignant B cell surface, designed for T cells to target B cells. It is a readily applicable product that can be administered without waiting for manufacturing, and patients can be treated without hospitalization. The administration duration is fixed to eight cycles. During this period, when a patient does not reach complete remission, the drug administration can be extended to 17 cycles. Professor Won Seog Kim of Samsung Medical Center's Hematology and Oncology said, "FL is considered a good type of lymphoma with a life expectancy of 20 years, but as patients experience repeated relapses, the disease becomes aggressive, and the prognosis worsens. Therefore, an effective treatment regimen with expected remission was urgent for patients with FL who have relapsed two or more times."
- Company
- Hope for polycythemia vera, Besremi, makes reimb progress
- by Eo, Yun-Ho Apr 21, 2025 05:53am
- Industry attention is gathering on the insurance reimbursement progress for the polycythemia vera treatment, Besremi. According to industry sources, PharmaEssentia Korea's new drug for polycythemia vera, Besremi (ropeginterferon alfa-2b-njft), has been determined cost-effective by the Health Insurance Review and Assessment Service's Pharmacoeconomic Evaluation Subcommittee. Accordingly, the procedure will proceed depending on whether the company accepts the government's proposal. As Besremi will gain a unique status in the field when listed, the industry expects the company and the government to derive positive results. This is the second attempt for Besremi’s reimbursement listing in Korea. In March 2023, the drug underwent the reimbursement process for refractory or intolerant polycythemia vera but failed to pass the Cancer Disease Review Committee in July of the same year. At the time, the Cancer Disease Review Committee determined that there was insufficient evidence to judge the clinical utility of Besremi as a second-line treatment. In response, PharmaEssentia resubmitted its application for reimbursement in March after adding domestic clinical data on Besremi and supplementing the evidence on the drug’s efficacy as second-line therapy, and the application passed CDDC review in July of the same year. At that time, the Cancer Disease Review Committee established the reimbursement standards for Besremi as a treatment for patients with polycythemia vera without splenomegaly accompanied by symptoms in low-risk groups (limited to patients requiring cytoreductive therapy) and high-risk groups. Besremi is a next-generation interferon treatment that selectively removes JAK2 mutations that cause polycythemia vera. It was developed to improve the purity and tolerability of existing interferons so that it can be administered every two weeks for the first 1.5 years and every four weeks thereafter. It is currently recommended for the treatment of PV in the National Comprehensive Cancer Network (NCCN) and European Leukemia Network (ELN) guidelines, regardless of prior treatment history. Polycythemia vera is a rare blood disorder where a somatic cell mutation in the bone marrow abnormally activates bone marrow function and produces excessive red blood cells. According to HIRA data, about 5,000 patients are affected with PV in Korea, and hydroxyurea is mainly used for the majority of patients. However, as the current reimbursed drugs are not curative and there are no new alternatives for patients who fail hydroxyurea treatment, there remains a high unmet need for the disease.
- Policy
- Comb cancer therapy issue has been resolved
- by Whang, byung-woo Apr 21, 2025 05:53am
- Changes will be brought to the health system as a patient's existing co-payment amount will remain the same for ongoing chemotherapy when a reimbursed cancer drug combined with a newly developed, non-reimbursed new drug. Previously, insurance coverage for combination therapy comprising two drugs was unavailable, placing a financial burden on patients. The recent changes to this policy are viewed positively. However, as more combination therapies with new drug-new drug combinations are being approved, there are discussions about the need to establish procedures. The Ministry of Health and Welfare (MOHW) has recently issued an administrative notice proposing partial revision to the 'Detailed Criteria and Methods for Applying Reimbursement (Drugs),' which included details on combination cancer therapy. Previously, if a non‑reimbursed drug was added to a regimen already covered by reimbursement, even the previously reimbursed drugs would lose their coverage, increasing patients' out‑of‑pocket costs. After the announcement, patient organizations and academics have proposed suggestions. In response, the Health Insurance Review and Assessment Service (HIRA) convened a Cancer Drug Review Committee (CDRC) meeting in October 2024 to establish a review policy for determining the reimbursement status of major combination therapies. Under the revisions, adding a non‑reimbursed anticancer drug to an existing reimbursed regimen will not affect the co-payment rate for the reimbursed drugs. In detail, a new clause states, 'When combining a reimbursed chemotherapy regimen with another anticancer drug, the existing co-payment for the previously initiated chemotherapy shall continue to apply to that regimen.' A pharmaceutical industry employee remarked, "The combination anticancer therapy included in this notice are first-line treatments that account for a relatively small share of the National Health Insurance expenditure, so there have been calls for improvement," and added, "We were expecting changes after the April 30 CDRC meeting, but it's good news to see the draft notification issued so quickly. From a pharmaceutical company perspective, this change is truly significant." The partial revision notice announced by the MOHW exemplifies the case of AstraZeneca’s immuno‑oncology drug Imfinzi (durvalumab), which was under discussion for biliary tract cancer reimbursement last year. At that time, the CDRC maintained Imfinzi as non‑reimbursed for first‑line treatment of biliary tract cancer while recognizing reimbursement only for the other combination therapy drugs, gemcitabine and cisplatin chemotherapy (GemCis). New drug+new drug combination therapy gains attention, demands for improving the reimbursement process↑ As issues for combination therapy comprising an existing first‑line chemotherapy agent with a new drug are likely to be resolved, interest is growing in whether a reimbursement process for "new drug + new drug" combinations can be established. In fact, with more multinational companies having applied for reimbursement of combination therapies that include innovative anticancer agents, requests for a formalized process have continued. According to discussions at the March 'Policy forum on improving cancer patient access to combination therapies,' 54 anticancer combination therapies have been approved in South Korea over the past five years. Of these, 28 cases add a new drug to an existing therapy, and 26 are combinations of two new drugs. In other words, roughly half of the recently approved combination therapies involve two novel agents. There are suggestions for institutional policies to ensure that reimbursement can be reviewed quickly and rationally when a combination therapy includes drugs from different companies. The Korea Research-based Pharmaceutical Industry Association (KRPIA) has formed a working group to devise solutions. (From left) Product photos of MSD Korea The government acknowledges the need to improve the system…limitations exist to mandating private companies A closer look reveals the challenges. When two new drugs from different companies are used for combination therapy, each company's circumstances, such as volume‑based pricing or price-volume agreement, make simultaneous reimbursement applications difficult. Currently, there is no basis for the two companies to coordinate their reimbursement status. If only one company applies, proving cost‑effectiveness can be problematic, and the therapy may remain split between reimbursed and non‑reimbursed drugs, contrary to the system's intent to reduce patient burden. While the government acknowledges the need for reforms, it also recognizes that it cannot mandate private pharmaceutical companies to comply. At the forum, Hee‑Yeon Park of the MOHW explained, "When combining new drugs+new drugs, we need additional measures. We are reviewing various approaches for reimbursement mediation, but there are aspects we cannot mandate due to each company's circumstances." Several ideas have been proposed similar to official notifications regarding generic drug pricing application cases. According to pharmaceutical industry sources, generics that enter the market after a delay instead of immediately after the patent expiry file for drug pricing review, HIRA will notify the original manufacturer, allowing the company to decide its response strategy. There is also a proposal to have HIRA notify other manufacturers when one company applies for an anticancer combination therapy reimbursement. Because companies do not publicly disclose their reimbursement applications, having HIRA coordinate and guide the review could aid in setting the directions. Additionally, experts have suggested applying a more flexible ICER threshold for combination therapies, recognizing that such regimens typically involve longer treatment durations than monotherapies. Therefore, proven innovative combinations should warrant a relaxed ICER criterion. A KRPIA official commented, "Several companies have agreed on the need to establish a clear process for combination therapy. We are gathering exemplary cases from abroad and will propose recommendations once we agree on the necessary steps."