- LOGIN
- MemberShip
- 2025-12-22 06:36:09
- Company
- Ebglyss may be prescribed in general hospitals in Korea
- by Eo, Yun-Ho May 16, 2025 06:21am
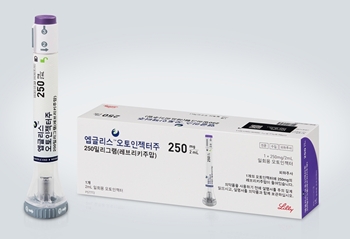
- Pic of Ebglyss The new drug Ebglyss for atopic dermatitis may be prescribed in general hospitals in Korea. According to industry sources, Lilly Korea's interleukin (IL)-13 inhibitor Ebglyss (lebrikizumab) has passed the Drug Committees (DCs) of 9 medical institutions nationwide, including tertiary hospitals like Asan Medical Center and Sinchon Severance Hospital, as well as Seoul National University Bundang Hospital. Accordingly, if Ebglyss is successfully listed for insurance reimbursement, the drug is expected to quickly lead to prescriptions. Lilly accepted a price below the evaluated amount (below the weighted average price of substitute drugs) presented by the Drug Reimbursement Evaluation Committee of the Health Insurance Review and Assessment Service in February and is currently negotiating Ebglyss’s drug price with the National Health Insurance Service. If listed, there will be 7 treatment options available for atopic dermatitis in Korea: biological agents (injectables) “Dupixent (dupilumab)” and “Adtralza (tralokinumab);” and JAK inhibitors (oral) “Rinvoq (upadacitinib),” “Civinqo (abrocitinib),” and “Olumiant (baricitinib).” The health authorities have recently been considering whether to allow JAK inhibitors to be used in cases where patients do not respond adequately to existing treatments (biological agents) or have poor tolerability, which is expected to further intensify market competition. If approved, Ebglyss will immediately benefit from the regulatory changes. The drug was approved by the Ministry of Food and Drug Safety in August 2024 for the treatment of moderate-to-severe atopic dermatitis in adults and adolescents 12 years of age and older (weighing at least 40 kilograms) who are inadequately controlled by topical treatments or for whom such treatments are not recommended. Ebglyss demonstrated its clinical efficacy and safety profile in a pivotal Phase III clinical trial. Patients who achieve a clinical response after 16 weeks of treatment can thereafter receive a maintenance dose (250 mg) every 4 weeks, making it a useful first-line treatment option for patients with atopic dermatitis in Korea. The clinical studies on which the license was based are the Phase III ADvocate-1, ADvocate-2, and ADhere trials. The trials evaluated the clinical efficacy and safety of Ebglyss in 1062 adults and adolescents with moderate-to-severe atopic dermatitis. In ADvocate-1 and ADvocate-2, which evaluated Ebglyss as a monotherapy, Ebglyss improved outcomes, with 58.8% and 52.1% (16.2% and 18.1%, respectively in the placebo arm) achieving Eczema Area and Severity Index (EASI) 75; and 38.3% and 30.7% (9% and 9.5%, respectively in the placebo arm) achieving EASI 90 during the induction period (weeks 0-16) compared to placebo. Also, after one year of maintenance therapy (Week 52), 81.7% of the Ebglyss arm achieved EASI 75 (vs. 66.4% in the placebo arm) and 66.4% achieved EASI 90 (vs. 41.9% in the placebo arm), demonstrating significant symptom improvement in the long term.
- Policy
- Trodelvy and new drugs reached an agreement with the NHIS
- by Lee, Tak-Sun May 16, 2025 06:21am
- Product photo of Trodelvy Three new drugs, including the triple-negative breast cancer (TNBC) treatment Trodelvy (sacituzumab govitecan), have completed negotiations with the National Health Insurance Service (NHIS) and are about to be included in the reimbursement list. These drugs passed the Health Insurance Review and Assessment Service (HIRA)'s Drug Reimbursement Evaluation Committee (DREC) in February and were undergoing negotiations with the NHIS. According to industry sources on May 15, the NHIS posted on its website that the companies of the TNBC drug 'Trodelvy,' the pulmonary hypertension drug 'Adempas Tab (riociguat, Bayer Korea),' and the plaque psoriasis drug 'Bimzelx Autoinjector (bimekizumab, UCB Korea)' have agreed on negotiation deals. During the 2nd DREC meeting on February 6, these drugs were acknowledged for their reimbursement appropriateness. The DREC granted reimbursement appropriateness for Trodevly's TNBC indication and Adempas' pulmonary hypertension among its efficacy·effectiveness. The efficacy·effectiveness of Adempas in chronic thromboembolic pulmonary hypertension (CTEPH) was not acknowledged for reimbursement appropriateness. For Bimzelx, the company received a decision that Bimzelx would meet the appropriateness of reimbursement if the company accepted an amount below the standard. After that, UCB accepted the condition and proceeded to negotiations with the NHIS. The company may have undergone negotiations with the NHIS for drug pricing and estimated claim amount, ultimately reaching an agreement. Among these drugs, Trodelvy received a decision of new drug innovativeness. It gained attention for becoming the first case to clear the DREC review, with its price being measured based on their ICER values. The Korea Alliance of Patients Organization (hereafter, Patients Organization) is asking for a quick reimbursement process since Trodelvy is the third-line treatment for adult patients with unresectable locally advanced or metastatic triple-negative breast cancer (mTNBC). The Patients Organization said, "Trodelvy is a high-cost drug, costing approximately KRW 1,500-2,000 per one cycle and some hundreds of millions of KRW yearly." They added, "Patients cannot continue treatment due to high-cost non-reimbursed drug costs and inevitably give up on receiving treatments." As these companies reached drug pricing negotiations with the NHIS, the drugs will be reviewed by the Health Insurance Policy Deliberation Committee. The drugs have higher chances of being included in the reimbursement list next month (June).
- InterView
- Hemlibra shows long-term efficacy and safety in hemophilia
- by Kim, Jin-Gu May 16, 2025 06:19am
- “The hemophilia patients’ only desire is to lead a normal life like everyone else. Hemlibra (emicizumab) has been found to be effective in preventing bleeding and safe in long-term follow-up studies. Moreover, it demonstrates clear bleeding prevention effects even during high-intensity exercise, significantly helping patients lead normal lives.” Dr. Steven Pipe, Professor of Pediatric Hematology-Oncology at the University of Michigan C. S. Mott Children's Hospital in the United States, said so while participating at the 'HAVEN Symposium' held on the 9th at the Sofitel Ambassador Seoul Hotel in Songpa-gu, Seoul. Dr. Pipe visited Korea to present the results of long-term administration of Hemlibra in patients with hemophilia A. He led the 'HAVEN3' and 'HAVEN4’ trials on Hemlibra. HAVEN3 is a study involving 151 hemophilia A patients who received emicizumab at a dose of 1.5mg/kg weekly or 3mg/kg every two weeks. HAVEN4 is a study involving 40 patients with hemophilia A who received emicizumab 6 mg every four weeks. Five years of follow-up data on the 191 patients showed that the annual bleeding rate (ABR) was 2.0 during the initial treatment period (weeks 1–24). At the long-term treatment stage (217–240 weeks), the annual bleeding rate fell to 0.8 episodes. Joint bleeds, a common complication in hemophilia A patients, also decreased in the long-term follow-up. The annual joint bleeding rate (AJBR) at the 217–240-week mark was 0.9 episodes. The proportion of patients who did not experience any bleeding during Hemlibra treatment increased from 62.2% at weeks 1–24 to 78.8% at weeks 217–240. Only 1 patient discontinued treatment over the five-year period. This case was a mild adverse reaction, and no association with the drug was identified. Twelve patients experienced inadequate bleeding control, and these patients continued treatment with an increased weekly dose of 3 mg/kg. Dr. Pipe highlighted the bleeding prevention effect of Hemlibra during various sports and physical activities. Similar to healthy individuals, he explained that there is little concern about bleeding even with high-intensity physical activity. The long-term follow-up results also showed that the annual bleeding rate (ABR) during sports and physical activities remained low at 0.91. Dr. Pipe said, “What hemophilia patients want most is ‘zero bleeding.’ They want to live their daily lives without any bleeding. Especially, they want to engage in high-intensity physical activities, including intense exercise, without worrying about bleeding.” In this sense, Hemlibra showed long-term efficacy as a preventive therapy. For example, at our hospital, 80% of patients diagnosed with hemophilia in childhood are currently receiving Hemlibra, and the drug shows definite bleeding prevention effects even during high-intensity exercise.” He also explained that the fact that Hemlibra maintains a higher level of clotting factor concentration for a longer period compared to existing treatments contributes to improving the patients' quality of life. Dr. Pipe said, “With previous medications, it was difficult to maintain consistent concentrations throughout the day, so patients had to take additional doses before intense exercise, which was inconvenient. In contrast, Hemlibra maintains consistent concentration levels, allowing patients to live their daily lives without such inconveniences.” Dr. Pipe plans to expand research on the long-term effects of Hemlibra in infants. He is conducting a long-term observational study (HAVEN 7) on the joint damage prevention effects of Hemlibra prophylaxis in 55 infants under one year of age with severe hemophilia A who have not developed antibodies to Hemlibra. R. Pipe stated, “Based on the results so far, infants receiving Hemlibra also exhibit a low annual bleeding rate. Even when bleeding occurs, it typically presents with traumatic bleeding patterns similar to those observed in infants of the same age. This is why we anticipate that Hemlibra will continue to demonstrate high bleeding prevention efficacy in the long term.”
- Policy
- CDDC to discuss partial reimb of anticancer drug combos
- by Lee, Tak-Sun May 16, 2025 06:18am
- The Health Insurance Review and Assessment Service announced today (14th) that it held a Cancer Disease Review Committee meeting and discussed the list of drugs eligible for partial reimbursement as anticancer drug combination therapies, as it had recently announced. The reimbursement standard for anticancer drugs will be revised starting next month based on the list made today. The details discussed at the meeting are expected to be disclosed when the reimbursement standard for anticancer drugs is announced. The Health Insurance Review and Assessment Service (President Jung-Gu Kang) announced that it had deliberated on the “Reimbursement Standards for Drugs Used for Cancer Patients” at the 4th Cancer Disease Deliberation Committee meeting in 2025. The details discussed on that day are follow-up measures to the revision of the general principles regarding “the scope and cost burden of drugs prescribed and administered to cancer patients among severely ill patients as drugs determined and announced by the Health Insurance Review and Assessment Service in accordance with Article 5, Paragraph 4 of the Rules on National Health Insurance Medical Care Benefits” among the details on the application criteria and methods for medical care benefits. At the meeting, the committee discussed the list of combination therapies eligible for reimbursement coverage, taking into account the indication and opinions from academic societies, with the aim of reducing confusion in clinical practice and enhancing predictability when applying the detailed guidelines to existing anticancer therapies and combination therapies with other anticancer drugs. The revised list will take effect on June 1. A total of 54 combination therapies were discussed, and 35 will be included in the revised guidelines. Therapies exceeding the approved indication were excluded. This decision was made as a minimum safety measure against the inappropriate use of combination therapies, such as those exceeding approved indications. The authorities explained that in the future, when academic societies submit requests for combination therapies related to this matter, the Cancer Disease Review Committee will review them and update the list of eligible therapies.
- Company
- AZ 'Imfinzi' leads the paradigm shift in cholangiocarcinoma
- by Whang, byung-woo May 16, 2025 06:18am
- "Introduction of Imfinzi in cholangiocarcinoma treatment can be seen as a critical advance. That a new therapy offering the possibility of long-term survival has appeared after 12 years is highly encouraging." As new treatment options for cholangiocarcinoma are introduced, a paradigm shift is said to be brought to this area, which was previously neglected and poorly developed. Although it is too early to be certain of long-term survival in South Korea, Dr. Yoo says that it could be a game-changer since new treatment options can benefit patient. Dr. Changhoon Yoo, Professor in the Department of Oncology at Asan Medical Center in SeoulDr. Changhoon Yoo, Professor in the Department of Oncology at Asan Medical Center in Seoul, who has expertise in this field, shared limitations in the treatment setting of cholangiocarcinoma and possible improvements. The prevalence of cholangiocarcinoma is known to be higher in Asia regions, including South Korea, China, and Taiwan, compared to Western countries. However, patients are often in advanced stages when diagnosed due to the challenging early diagnosis. It is one of the cancers that is difficult to reach a curative intent. Dr. Yoo explained, "Cholangiocarcinoma has a low prevalence due to its high mortality, resulting in a low cumulative patient number relative to its incidence. Currently, only about 20–30% of cholangiocarcinoma patients are eligible for surgery, and the remaining approximately 70% must rely on drug treatments such as chemotherapy or immunotherapy." While liver fluke infection was the leading cause of cholangiocarcinoma in the past, new factors such as fatty liver have emerged due to the westernization of dietary habits. 임핀지(더발루맙)After Imfinzi (durvalumab) received approval from the Ministry of Food and Drug Safety in November 2022, it is continuously expanding its influence. Dr. Yoo said, "Although less than three years have passed since the indication approval and it is therefore difficult to confirm long-term survival rates, in clinical practice the proportion of patients showing improvement has increased compared with before," adding, "Considering that patients who received Imfinzi combination therapy early in the 2021 clinical study still have favorable outcomes, Imfinzi can be seen as providing benefits to patients." In particular, Dr. Yoo focused on Imfinzi's side effects and safety. Dr. Yoo explained, "Most side effects are caused by the cytotoxic chemotherapy agents used in combination, and there are almost no issues attributable to Imfinzi. It rarely causes patients to struggle or reduces clinical efficacy, making it a medication that is of considerable help not only to patients but also to healthcare providers." "Korean subgroup analysis data on Imfinzi demonstrates long-term survival effects" Another reason why Imfinzi combination therapy is gaining attention in cholangiocarcinoma is that overall survival (OS) was shown to be higher in Korean patients. According to the study results, the two-year survival rate in the Korean patient group receiving the Imfinzi combination therapy was 38.5%, more than twice the 14.1% observed in the group that received chemotherapy. Furthermore, the survival rate at 36 months was 21.0% in the Imfinzi combination group, more than double the 8.8% in the chemotherapy group. Dr. Yoo analyzed, "In my opinion, I consider the Korean subgroup analysis data from the TOPAZ-1 study very encouraging. These results reflect the rapid accessibility and thorough patient management within the healthcare system." In cholangiocarcinoma, where inflammation or adverse reactions often occur during anticancer treatment, leading to treatment interruptions and repeated hospital admissions and discharges, continuous cancer treatment itself is challenging. According to Dr. Yoo, it is particularly common for treatment to be paused for a month or two due to inflammation, worsening the disease, and cholangitis can occur even when the cancer itself is not progressing. Therefore, high accessibility to treatment is critical in cholangiocarcinoma. Dr. Yoo said, "In Korea, if inflammation or jaundice occurs, patients can quickly visit a hospital, receive a procedure, and recover, thereby immune checkpoint inhibitors can be administered continuously," and added, "Compared to countries with less-established healthcare systems, our accessibility and level of care are higher, so I believe the effectiveness of immune checkpoint inhibitors can be more pronounced." Dr. Yoo also said, "Cholangiocarcinoma is indeed a challenging disease, but prognosis has improved recently and long-term survival cases are increasingly common," and added, "To secure approval or reimbursement for new drugs, one side's opinion is not enough. It is also necessary for patients and healthcare professionals to raise their voices together." Reimbursement discussions remaining for Imfinzi combination Therapy… "The standard criteria application should be avoided" However, the Imfinzi combination therapy is only reimbursed for the chemotherapy, and the cost barrier remains high. Currently, Imfinzi's reimbursement criteria were established in November of last year. Following AstraZeneca Korea's application for the cost‐effectiveness track, the Health Insurance Review and Assessment Service (HIRA)'s Economic Evaluation Committee is expected to discuss Imfinzi's cost‐effectiveness this month. According to industry sources, this month's Economic Evaluation Committee will review the cost‐effectiveness of Imfinzi+gem-cis combination therapy as a first‐line treatment for locally advanced or metastatic cholangiocarcinoma. It will be forwarded to the Drug Reimbursement Evaluation Committee if it passes the Economic Evaluation Committee. In this regard, Dr. Yoo noted that, for the sake of patient access, the standard criteria should be avoided. For example, in hepatocellular carcinoma, the standard treatment, sorafenib, is not particularly low‐cost, so its price could not be matched when a new drug emerged. Still, it is disadvantageous for a new drug to meet such price benchmarks for rare diseases or those where drug development has lagged. Dr. Yoo said, "When nanoliposomal irinotecan was introduced as a second‐line treatment for pancreatic cancer, it also faced challenges in economic evaluation when compared with 5‐FU." And added, "Likewise, I do not think conducting a straightforward economic comparison between existing cholangiocarcinoma drugs, whose patents have expired and thus are inexpensive, and an innovative new drug developed after a decade is appropriate." Dr. Yoo also described cholangiocarcinoma as 'the lung cancer of the gastrointestinal cancer family,' emphasizing the importance of precision medicine in new drug development. "Although cholangiocarcinoma has one of the poorest prognoses among gastrointestinal cancers, I am interested in the possibility of developing targeted therapies based on genetic analysis of specific biomarkers," Dr. Yoo added, "Approximately 4–5% of cholangiocarcinoma patients carry specific gene mutations, making this a cancer type with high potential for precision‐medicine application, and research is underway." Finally, Dr. Yoo urged, "Support for precision medicine and targeted‐therapy development is urgently needed to broaden patient treatment opportunities." And, "I hope that cholangiocarcinoma patients will not lose hope and will actively pursue their treatments."
- Policy
- Gov't begins patient advocacy service for medical incidents
- by Lee, Jeong-Hwan May 15, 2025 06:24am
- The Korean Ministry of Health and Welfare (MOHW)The Ministry of Health and Welfare (MOHW) will start implementing the 'patient advocacy service,' which provides a legal representative matching service for mediating disputes to strengthen the rights of patients who are victims of medical incidents, effective this month (May). The service supports the conflict between a patient and a medical institute·healthcare provider. The MOHW will initiate the program on the 16th by appointing approximately 50 lawyers. The patient advocacy service will include patients who are victims of medical incidents during surgical operations and prescription·drug preparation errors that occur in hospitals. During the meeting with the Korea Special Press Association on May 14, Minjung Kwon, Director of MOHW's Healthcare Institution Policy Division, stated this. Medical incident patient advocacy service is related to the MOHW's 'Act on Special Cases Concerning Medical Accident,' which was part of the essential healthcare package. The 'Special Act for Handling Medical Accident' exempts criminal punishment of doctors when accidents occur during medical practice in essential healthcare departments. Accordingly, patient·citizen organizations shared criticism that the act invades the patient's rights while maximizing doctors' benefits. The MOHW has established a patient advocacy service for medical incidents to safeguard patient rights. To carry out this plan, the MOHW has completed the selection of patient advocates, focusing on lawyers with experience in medical malpractice litigation, among those who are both lawyers and hold medical licenses, and individuals with expertise and experience in medical accidents. The patient advocacy service is activated·operated during the dispute mediation stage before or instead of proceeding to court when a medical accident occurs. Patients who wish to use the advocate system must apply to the Korea Medical Dispute Mediation and Arbitration Agency. The MOHW plans to implement the patient advocate system as a provisional program while preparing the legal basis for it in the future. Director Kwon explained, "Many lawyers applied for the patient advocate service," and added, "We aimed to select around 50 people, but received more applications. After the appointment ceremony on the 16th and the training course, we plan to start the service at the end of May." "This is a program in which patients who wish to apply for medical accident mediation can apply to the advocate system, receive assistance, and proceed with mediation together," Director Kwon added, "The advocacy service is not intended for patients who want to file law suits. If mediation is activated through the advocate system, reducing cases that proceed to law suits will be possible." Lastly, Director Kwon said, "The term for a patient advocate is two years. After two years, performance will be evaluated, and reappointment will be made if no special circumstances exist." And added, "Many lawyers are interested in public service and have applied for this system. We intend to encourage advocates' participation and develop these various medical dispute mediation and assessment systems together."
- Opinion
- [Reporter's View] Korea’s vaccination space: ups and downs
- by Eo, Yun-Ho May 15, 2025 06:23am
- Vaccines are at the forefront of localized pharmaceuticals in Korea. Leading domestic companies such as GC Biopharma and SK Bioscience are now responsible for vaccine production and supplying preventive vaccines for various diseases, including influenza. The commercialization of so-called “premium homegrown vaccines,” such as pneumococcal protein vaccines, cervical cancer vaccines, and shingles vaccines, is also progressing steadily and is set to be completed soon. However, despite the improvement in vaccine competitiveness, the vaccination fee cartel among doctors in South Korea remains unchanged. For example, if the purchase price of a vaccine (the price at which doctors buy vaccines from pharmaceutical companies) is KRW 100,000, the implicitly accepted appropriate inoculation fee among doctors is around KRW 200,000. However, after some time passes, some local clinics lower the vaccination fee to as low as KRW 150,000 in an attempt to sell more at lower prices. Some even abandon their margins altogether, offering even lower prices through promotional events. These clinics then face criticism from neighboring doctors. They are labeled as traitors who betrayed their colleagues for their own gain. Such controversies can escalate into disputes between different medical specialties. The medical society of the relevant specialty may launch a campaign claiming that people should be vaccinated by specialists in their respective field. The interesting point lies in the margins. For vaccines, the difference between the inoculation fee and the purchase price, minus approximately 30% tax, constitutes the doctors' income. If they receive the “appropriate price” they claim—KRW 200,000 per vaccination—the actual income may vary depending on tax reporting, but amounts to roughly 70,000 won. For some workers, this is equivalent to a day's wage. Even if they receive KRW 150,000, approximately KRW 35,000 margin remains. This is by no means a small amount. Private practitioners claim that after including vaccination fees and labor costs, nothing remains. Meanwhile, during the flu season, they engage in fierce competition to secure supplies of flu vaccines, where the purchase price is KRW 10,000, and an approximately KRW 12,000 margin remains per inoculation. Private practice doctors are self-employed. This is a fact. Therefore, it is understandable that they want a high income that commensurates with the effort they put into obtaining their medical license. Additionally, since vaccine prices are not fixed, they have the right to set their own prices. However, they should refrain from claiming that twice the purchase price is the “appropriate price” and form a cartel. I earnestly hope they will finally “recognize” that the era when doctors' words were unquestioningly accepted is now over.
- Company
- Doctors ‘Reimb too slow for new drugs in Korea’
- by Eo, Yun-Ho May 15, 2025 06:23am
- Most doctors were found to believe that the speed of reimbursement for new drugs in Korea is too slow. The Korean Research-based Pharmaceutical Industry Association (KRPIA) released the results of a survey of 100 domestic medical professionals on the 14th. In January, the global polling agency Ipsos Research surveyed domestic clinical experts from various medical departments to ask their opinions on access to new drugs. According to survey results, all medical professionals unanimously answered that the period from the Ministry of Food and Drug Safety approval to health insurance reimbursement listing is “long,” with 74% stating it is “too long.” Regarding the appropriate period from approval to health insurance listing, 81% of medical professionals answered “up to 10 months,” with 41% deeming “within 6 months” as appropriate. As of 2022, it takes an average of 608 days (approximately 20 months) for innovative new drugs to be approved by the MFDS and listed for health insurance reimbursement in Korea. This is twice the appropriate period cited by most medical professionals (10 months) and significantly longer than in major overseas countries such as Germany (281 days), Japan (301 days), and France (311 days) during the same period. Furthermore, experts directly treating patients in the clinical settings anticipate that the swift and widespread introduction of innovative new drugs will provide substantial benefits for patient care. Eighty-three percent of medical professionals expected that “if drugs already in common use overseas are covered by health insurance in Korea, patient treatment outcomes will improve significantly.” A large proportion of medical professionals (85%) responded that “even for drugs already covered by health insurance, if reimbursement standards are eased to enable early or wider use, patient treatment outcomes will improve significantly.” In addition, 95% of medical professionals urged the MOHW to introduce a “fast-track listing procedure or system” for health insurance coverage, similar to the MFDS's Global Innovate Products on Fast Track (GIFT) system, which shortens the drug approval review period for severe or life-threatening diseases by up to 75%. Medical professionals who participated in the survey also expressed concerns about Korea's low access to new drugs. Ninety-four percent of medical professionals pointed out that “Korea's access to new drugs is lower than overseas,” and 97% answered that “the government must set appropriate and reasonable drug prices to prevent the ‘Korea passing’ phenomenon, where multinational pharmaceutical companies give up the launch of innovative new drugs in Korea due to domestic regulations on pharmaceuticals.” Seventy-six percent of medical professionals were concerned that the proportion of new drug expenditures (13.5%) in total domestic drug expenditures is 60% lower than the OECD average (33.9%), and 88% believed that reimbursement and access to new drugs in South Korea need to be improved to the level of the top 10 OECD countries. Medical professionals identified “enhancing access to innovative new drugs” as the top priority among the four key strategies of the government's Second Comprehensive National Health Insurance Plan (2024-2028). As the government pushes policies to reduce drug costs in response to an aging society, 67% of medical professionals expressed the view that “the budget savings should be reinvested into the health insurance fund.” As the survey respondents were clinical experts, they also requested that the opinions of those working on-site be more actively taken into account in the reimbursement decision-making process. Eighty-eight percent of medical professionals responded that “the opinions of medical professionals should be better reflected in the process of registering drugs for health insurance coverage,” and 80% said that “medical professionals should also be involved in the process of selecting patient population eligible for health insurance coverage.” A KRPIA official stated, “Medical professionals who care for patients on the front lines are deeply concerned about the difficulties patients face in receiving treatment due to delays in the introduction of innovative new drugs. They hope that new drugs will be listed for health insurance reimbursement more swiftly and with a broader scope. We anticipate that the results of this survey will contribute to the government’s fostering of a patient-centered treatment environment and policy design.”
- Company
- Arexvy opening the era of RSV vaccine
- by Whang, byung-woo May 15, 2025 06:22am
- As GSK launches the respiratory syncytial virus (RSV) vaccine Arexvy in South Korea, it will challenge the market on a full-scale. Arexvy is already expanding its market dominance in the global market with its strength as the first RSV vaccine. The company will likely focus on expanding vaccine awareness as it opens the RSV vaccine market for the first time. Dr. Ji-Yong Moon, Professor of Konkuk University On May 14, GSK Korea convened a press conference celebrating the launch of Arexvy, the world's first RSV vaccine. The company showcased a preventative strategy for seniors against RSV and Arexvy's clinical significance. Arexvy received approval from the Ministry of Food and Drug Safety (MFDS) at the end of December 2024 for the 'Prevention of lower respiratory tract disease (LRTD) caused by RSV in adults over 60 years of age and older.' Approval of Arexvy was based on results from two Phase 3 studies, 'RSV OA=ADJ-006' and 'RSV OA=ADJ-004,' involving adults 60 years of age and older. The study results showed that during the first RSV season, Arexvy significantly lowered the RSV-LRTD risk by 82.6% and severe RSV-LRTD risk by 94.1% in participants 60 years of age and older compared to placebo. Furthermore, the efficacy of the vaccine regarding RSV-A-associated LRTD increases and RSV-B-associated LRTD increases were 84.6% and 80.9%, respectively. Dr. Ji-Yong Moon, Professor of Konkuk University's Department of Respiratory-Allergy and Clinical Immunology, explained, "RSV infection causes complications, such as pneumonia, in adults aged 60 years or older and it may require hospitalization or lead to death in severe cases," and added, "Based on a retrospective study, 56.8% of the hospitalized adults over age of 65 had pneumonia and 10.6% of those died." Dr. Moon added, "Despite the high disease burden, awareness of RSV infection is poor, and differential testing is not well implemented, so the disease burden of RSV infection has been underestimated." He said, "RSV infection is as contagious as influenza, but there is no specific treatment other than supportive care, so prevention is most important." (from left) Professor Jacob Lee, Professor of the Division of Infectious Disease at Hallym University Kangnam Sacred Heart Hospital, and, Dr. Ji-Yong Moon, Professor of Konkuk University Experts consider that the launch of the first RSV vaccine, Arexvy, is expected to be significant from a preventive standpoint. Professor Jacob Lee, Professor of the Division of Infectious Disease at Hallym University Kangnam Sacred Heart Hospital, reported that RSV vaccination is already recommended in the United States. Dr. Lee said, "Arexvy showed a preliminary efficacy of 94.6% against RSV-LRTD in adults with one or more comorbidities," and emphasized, "Considering that 84% of domestic adults aged 65 and over have one or more chronic diseases, these data are noteworthy." Dr. Lee stated, "Arexvy was approved in the U.S. in 2023, real-world data on its use have accumulated, and excellent preventive efficacy has been confirmed in actual clinical settings." He said, "The U.S. Advisory Committee on Immunization Practices (ACIP) recommends RSV vaccination for high-risk individuals aged 60–74 and all adults aged 75 and older." Cost and awareness remain challenges… "NIP is necessary from a long-term perspective" Regardless of the preventive value of RSV through Arexvy, it remains uncertain how much influence it will exert in the market. Currently, Arexvy remains non-reimbursed in South Korea. Without a recommendation like that of the U.S. ACIP, there is a need to improve awareness. In particular, the fact that the recommended vaccination age in the U.S. is higher at 75 years old, compared to the domestic approval age of 60 and over, also raises questions. Hyunji Kwon, Business Unit Head at GSKRegarding this, Dr. Lee explained, "In South Korea, the Korean Society of Infectious Diseases is expected to announce a recommendation within this year, but it is unlikely to differ significantly from the U.S.," and added, "To enter the National Immunization Program (NIP), sufficient disease burden research needs to be conducted." Dr. Lee continued, "There is a cost burden and domestic data are lacking, but as the population structure changes, the number of vaccination targets will also increase. Through research data and cost-effectiveness, we can hope for RSV prevention through the NIP in the long term." GSK Korea has stated that it will work to improve awareness through TV advertisements and other means alongside the launch of Arexvy. Hyunji Kwon, Business Unit Head at GSK, added, "RSV is a disease with a great unmet medical need yet remains unfamiliar, so we will work to improve awareness among medical staff and high-risk patients," and added, "In a super-aged society in which, for the first time, the population in their 60s exceeds that in their 40s, we will collaborate with the medical community and the government to increase patient access."
- Company
- Will a new trend emerge for liver cancer treatment?
- by Moon, sung-ho May 15, 2025 06:22am
- With new anticancer drugs entering the liver cancer treatment market, where combination therapy has been gaining prominence, attention is focused on whether a paradigm shift will occur. This is because a new competitive landscape is forming with the arrival of newly approved drugs and newly reimbursed drugs. # According to industry sources on the 7th, the US Food and Drug Administration (FDA) recently approved the combination therapy of Bristol Myers Squibb (BMS) and Ono Pharmaceutical's Opdivo (nivolumab)+Yervoy (ipilimumab) combination as a first-line treatment for adult patients with unresectable or metastatic hepatocellular carcinoma (HCC). The approval was based on the results of a randomized, open-label, global Phase III clinical trial (CheckMate-9DW) comparing the combination therapy of Opdivo and Yervoy (335 patients) with either lenvatinib or sorafenib monotherapy (333 patients). The trial was conducted on patients with unresectable or metastatic HCC who had not previously received systemic therapy. The CheckMate-9DW results showed that the median overall survival (mOS) in the Opdivo+Yervoy combination therapy group was 23.7 months (95% CI: 18.8-29.4), compared to 20. 6 months (95% CI: 17.5-22.5) in the control group (n=333), reducing the risk of death by 21% (HR=0.79; P=0.0180). In addition, the 3-year survival rate was 38% in the Opdivo+Yervoy combination therapy group, higher than the 24% in the control group. The objective response rate (ORR) was also significantly higher in the combination therapy group at 36.1% (95% CI: 31–41.5) compared to 13.2% (95% CI: 9.8–17.3; P