- LOGIN
- MemberShip
- 2025-12-22 06:36:13
- Company
- ‘Multiple-indication drugs improve survival rates’
- by Son, Hyung Min Apr 28, 2025 05:54am
- Hosted by KRPIA The Korean Research-based Pharmaceutical Industry Association (KRPIA) announced on the 24th that it successfully hosted a “Policy Forum on Eliminating Inequality in Innovative New Drugs and Improving Regulations” with Representative Mi-hwa Seo, Representative Byeong-Hoon So, Representative Yoon Kim, and Representative Jong-tae Jang (Health and Welfare Committee) of the Democratic Party of Korea. The policy forum, held at the National Assembly Office Building, aimed to explore measures to improve access to innovative new drugs for patients with severe and rare diseases so they can receive timely treatment, and to gather opinions from various sectors. The symposium was attended by co-hosts Rep. Mi-hwa Seo and Rep. Yoon Kim, as well as keynote speakers Jung-yong Hong, Professor of Oncology at Samsung Medical Center, and Professor Jung-hoon Ahn, Professor of Health Convergence at Ewha Womans University. The discussion panel included key figures from the government, the medical community, patient groups, the media, and the pharmaceutical industry, such Lee Jung-kyu as, Director of the Health Insurance Policy Division at MOHW; Hyung-min Kim, Director of the Department of Drug Management at the National Health Insurance Service; Ji-yong Moon, Professor at Konkuk University Medical Center; Gi-jong Ahn, Representative of the Korea Alliance of Patients Organization; Yoonho Eo, reporter at Dailpyharm; and Hyeryun Bang, Director at AstraZeneca Korea. The discussion was moderated by Dong-Cheol Seo, Director of the Korea Institute for Pharmaceutical Policy Affairs. In her opening remarks, Rep Mihwa Seo said, “When patients miss their chance for treatment, the costs go beyond simple medical losses and become enormous social costs,” emphasizing that “the fundamental reasons for the low accessibility of new drugs in Korea lie in the rigidity of the overall system, including the procedural complexity of the reimbursement listing system, the economic evaluation-centered assessment model, and the uniform drug price structure. The government must assume a responsible role in addressing all factors that have a substantial impact on patients' lives.” In his greeting, KRPIA Chair Kyung-Eun Bae said, “New drugs with multiple indications greatly contribute to improving patient survival rates and quality of life, but their value is not fully reflected due to the structural limitations of the domestic reimbursement system. I hope that patients' treatment opportunities will be expanded by reflecting the differences in therapeutic effects, number of patients, and availability of alternative treatments for each indication, even for the same drug.” In his keynote speech, Jung-yong Hong, Professor of Oncology at Samsung Medical Center, addressed the structural issues of clinical value and accessibility imbalances in innovative new drugs under the theme of “Regulatory Improvement Tasks for Addressing Inequality and Improving Accessibility of Innovative New Drugs in Korea.” He pointed out that innovative new drugs with different mechanisms of action from existing treatments are effective for various indications, meet unmet medical needs, and have received high prescription recommendation ratings in global guidelines, but patients in Korea are unable to obtain actual treatment opportunities due to limitations in the reimbursement system. In particular, he mentioned that reimbursement for drugs with multiple indications is delayed compared to other countries and raised the need for policy attention and institutional reform to improve accessibility. In the second presentation, Jung-hoon Ahn, Professor of Health Convergence at Ewha Womans University, emphasized the need for a value-based drug pricing system, focusing on the fact that the therapeutic effects and social value of drugs vary depending on their indications. For this, Ahn introduced the “blended pricing” system, in which drug prices vary depending on the number of patients, the availability of alternative treatments, and cost-effectiveness, even for the same drug. He explained that this system, which is already in place in several countries, could serve as an alternative solution that not only reflects the value and usage of each indication but also enhances the sustainability of health insurance finances and patient access. The subsequent panel discussion delved into in-depth discussions on field experiences and potential institutional improvements. Gi-jong Ahn, Representative of the Korea Alliance of Patients Organization, said, “It is difficult for patients to understand why certain indications are not covered by health insurance and therefore cannot be used. Despite financial concerns, considering the examples of countries that have introduced blended pricing systems, South Korea also needs to consider introducing such a system quickly and improve access to treatment. Jung-kyu Lee, Director of the Health Insurance Policy Division at MOHW, said, “Many newly approved drugs have multiple indications,” adding, “The government agrees that it is time to review the blended pricing system.” He added, “We will carefully examine whether this is a problem with existing practices or a limitation of the system, and if there are systemic problems, the health authorities will comprehensively review and discuss improvement measures with the Health Insurance Review and Assessment Service and the National Health Insurance Service.” Hyung-min Kim, Director of the Department of Drug Management at the National Health Insurance, said, “Careful system design is required based on financial stability, patient accessibility, and connectivity with other systems.”
- Company
- Janssen’s Rybrevant challenges the NSCLC throne
- by Whang, byung-woo Apr 25, 2025 05:59am
- The Rybrevant-Leclaza combination therapy, which has emerged as the standard of care in the field of lung cancer, is set to enter the market in earnest, backed by clinical data. With three additional indications for EGFR-mutated non-small cell lung cancer added this year, the company plans to leverage its leadership in the field of lung cancer. Kihyung Lee, Professor of Hemato-oncology at Chungbuk National University HospitalOn the 22nd, Janssen Korea held a press conference to highlight the indication expansion of Rybrevant (amivantamab) and the clinical value of its combined use with Leclaza (lazertinib). Results of 3 major Phase III clinical studies of Rybrevant in the treatment of EGFR-mutated non-small cell lung cancer were shared at the conference. Kihyung Lee, Professor of Hemato-oncology at Chungbuk National University Hospital, who presented at the event, said, “A significant number of patients with EGFR exon 19 deletion and exon 21 (L858R) substitution mutations experience resistance during treatment with existing EGFR-TKIs, with limitations in selecting subsequent treatment options.” He added, “Rybrevant has presented a new treatment method for EGFR-mutated non-small cell lung cancer through the use of combination therapy.” Rybrevant is the first targeted therapy for EGFR exon 20 insertion mutation non-small cell lung cancer, and it not only targets EGFR exon 20 insertion mutations but also simultaneously targets MET mutations. Professor Lee said, “Rybrevant inhibits tumor growth and progression by suppressing tumor cells that show not only EGFR mutations but also MET mutations and amplification. It also has a differentiated mechanism of action that induces cancer cell death through immune mechanisms such as natural killer cells and macrophages.” Rybrevant + Leclaza shows improvement in OS following PFS The basis for adding the new indication for Rybrevant in EGFR-mutated non-small cell lung cancer was 3 Phase III clinical studies: MARIPOSA-1, MARIPOSA-2, and PAPILLON. According to the final results of the MARIPOSA Phase III clinical study presented at the European Lung Cancer Congress (ELCC 2025) held in March, showed that the combination therapy of Rybrevant and Leclaza was superior to Tagrisso monotherapy. The MARIPOSA study is a clinical trial comparing the efficacy and safety of Leclaza + Rybrevant combination therapy with Tagrisso monotherapy, which is currently used as a first-line treatment for EGFR-positive non-small cell lung cancer. The clinical results showed that the median progression-free survival (PFS) in the Leclaza+Rybrevant group was 23.7 months, which was longer than the 16.6 months recorded in the monotherapy group. In the analysis of overall survival (OS), the secondary endpoint, the Leclaza+Rybrevant group showed a favorable trend compared to the Tagrisso monotherapy group. Se-Hoon Lee, Professor of Hemato-oncology at Samsung Medical Center Se-Hoon Lee, Professor of Hemato-oncology at Samsung Medical Center, said, “At a median follow-up of 37.8 months, the Rybrevant combination showed a significant improvement in OS compared with osimertinib monotherapy.” He added, “The objective response rate of Rybrevant was 86% in patients with EGFR exon 19 deletion and exon 21 substitution mutations, and the median duration of response was 25.8 months, which means that combination therapy with Rybrevant can be considered a major treatment strategy.” With Leclaza + Rybrevant confirming its superiority in OS, the EGFR-positive non-small cell lung cancer treatment market is now likely to see combination therapy become the standard treatment. Currently, this combination therapy has been approved as a first-line treatment in South Korea, the United States, Europe, Japan, the United Kingdom, and Canada. Particularly, while combination therapy that combines platinum-based chemotherapy with targeted therapy has been approved for EGFR-positive NSCLC in the past, this is the first time a targeted therapy+targeted therapy option has been approved, signifying its significant development. More options available for EGFR-positive NSCLC, but tailored selection remains a challenge However, despite the combination rising as a possible standard treatment, there are cost barriers to its immediate use in clinical practice. With four options now available, including monotherapy and combination therapy, determining the optimal sequence of treatment is also a key consideration. Professor Lee said, “It is a difficult issue, but with 100 patients that all have different characteristics, I think their conditions must be taken into consideration. Rather than categorizing specific groups, I expect that the most beneficial treatment for each will be selected according to each patient's condition.” In addition, Janssen Korea expressed its commitment to improving access to combination therapy with Rybrevant. Yeon-hee Kim, Oncology Business Unit Director at Janssen Korea, added, “We are making various efforts to expand access to Rybrevant combination therapy. We will do our best to ensure that health insurance reimbursement coverage is provided through flexible and active cooperation during the reimbursement review process.”
- Policy
- ‘Should apply blended pricing and reimbursement rates’
- by Lee, Jeong-Hwan Apr 25, 2025 05:59am
- With multiple drugs with multiple indications, such as multi-targeted immunotherapy drugs, being approved in Korea, there have been claims that the introduction of an “indication-based drug pricing system” is necessary to improve patient access to treatment and ensure equity. In particular, the argument was made that ‘blended pricing,’ which sets different prices for each indication, could reflect the value of each indication while maintaining a single price, thereby increasing social acceptability, and that it could be introduced without conflicting with the current drug pricing system in Korea, which is based on a single price structure. Ultimately, after taking the first step with “blended pricing,” the industry recommended that the government should introduce a “differentiated reimbursement rate system” based on real-world data accumulated for each indication in order to reflect the value of drugs for each disease and speed up reimbursement for patients. Jung-hoon Ahn, Professor of Health Convergence at Ewha Womans University Graduate School, will present these views at a policy discussion forum titled “Resolving Inequality in Innovative New Drugs and Regulatory Reform” co-hosted by the Democratic Party of Korea lawmakers Mihwa Seo, Byung-Hoon So, Yoon Kim, and Jong-Tae Jang on the 24th. The forum is organized by the Korean Research-based Pharmaceutical Industry Association (KRPIA). Professor Ahn will give a presentation on the reimbursement policy for drugs with multiple indications. Professor Ahn pointed out that there are an increasing number of cases in which drugs with multiple indications are being approved in the field of anticancer drugs. In fact, as of 2018, 75% of tumor treatment drugs in the United States were approved as drugs with multiple indications, and in South Korea, 32 anticancer drugs with multiple indications are eligible for reimbursement. In South Korea, drug prices are determined based on the active pharmaceutical ingredient contained in the drug, making it difficult to set and reflect separate prices for individual indications. This means that even drugs with multiple indications are assigned a single insurance reimbursement ceiling. Professor Ahn expressed concerns that the value of individual indications is not sufficiently reflected in drug prices, leading to issues such as access to treatment for patients that are covered with the expanded indications in South Korea. Taking the multi-indication immunotherapy drug Keytruda as an example, he pointed out that while it is reimbursed in Italy, Switzerland, France, Australia, Japan, and Belgium for both first-line treatment of head and neck squamous cell carcinoma and second-line treatment of endometrial cancer, it is not reimbursed for either in South Korea. In response, Professor Ahn suggested the need to introduce or improve a drug pricing system for multi-indication drugs. Specifically, Professor Ahn proposed that while methods such as “individual approval for each indication” or “differentiated reimbursement rates” could transparently reflect the value of each indication, they require legal amendments or raise concerns about equity in reimbursement amounts between patients that are applied different indications, as well as the need for preparation in the current system, including settlement mechanisms. He emphasized that the blended pricing method is highly feasible under the current reimbursement and drug price system. The logic is that applying blended pricing within the framework of risk-sharing agreements (RSAs), which are legal contracts, would allow the value of drugs to be reflected according to their indications while managing the financial risk of drugs with uncertain cost-effectiveness. Professor Ahn stated, “The country has established a value-based drug pricing system. However, while value is recognized primarily based on the primary indication, appropriate values for individual indications are not reflected. As a result, pharmaceutical companies are delaying or abandoning the launch of subsequent indications, leading to reduced access to new treatments for patients.” “I propose collecting and analyzing real-world data on claims made for each indication to establish actual value evidence for drugs, and building a system that applies differential reimbursement rates that reflect the clinical value differences by indication based on accumulated data,” said Ahn. “This is a strategic approach that complements the limitations of Korea's single drug pricing system while flexibly realizing the effects of indication-based drug price adjustments.” He added, “We can start with a practical approach, such as blended pricing (indication-weighted average price), and gradually evolve toward a differentiated reimbursement rate system that reflects indication-specific value. Blended pricing maintains a single price while reflecting the value of individual indications, making it more acceptable within the social framework.”
- Policy
- "Will consider proposal for Indication-based pricing system"
- by Lee, Jeong-Hwan Apr 25, 2025 05:58am
- Lee Joongkyu, Director of the National Health Policy at the Ministry of Health and Welfare (MOHW), at the National Assembly policy forum Regarding introducing an 'indication-based pricing system' aimed at improving patient access to medications, Lee Joongkyu, Director of the National Health Policy at the Ministry of Health and Welfare (MOHW), stated, "While it is still too early to announce when to implement the system, it is an opportune time to consider reviewing the proposal." During the 'Discussion Forum on Resolving Inequalities in Innovative New Drugs and Regulatory Reforms' at the National Assembly on April 24, Director Lee explained, "Recently, multiple indications are frequently approved for new drugs, thus presenting issues that cannot be solved in previous methods." Director Lee highlighted that the National Health Insurance's operational direction is to provide medications that citizens need in a timely manner. In other words, introducing an indication-based pricing system aimed at improving patient access to medications still requires further discussion within the Ministry of Health and Welfare (MOHW). Directior Lee said that since the Korean health insurance system operates as a sole supplier than a multiple insurance system, there will be challenges related to purchasing medications and receiving reimbursement. Despite such challenges, Director Lee agreed that solving the patient access issue by improving policy is necessary rather than simply regarding it as a financial issue. Dr Lee remarked, "We must consider whether issues related to reimbursement method of pharmaceutical have been resulted due to insufficient measures from the perspective of the system rather than a National Health Insurance expenditure issue," and added, "In my opinion, it is about time to review the indication-based pricing system." "We cannot provide an exact implemenation timeline, but the MOHW will review the measure. The MOHW is aware that if coverage under the National Health Insurance is not provided, individuals will need to purchase medications at non-reimbursed price," and Dr. Lee added, "If there are issues with the supply of quality drugs, we will certainly consider proposals."
- Policy
- MFDS to improve essential drug designation standard
- by Lee, Hye-Kyung Apr 25, 2025 05:58am
- The Ministry of Food and Drug Safety will conduct a study to improve the standards for designating essential medicines. When the national essential medicine system was first implemented in 2017, the designation focused on government stockpiles, but there have been continuous calls to expand the list to include items that require stable supply in the private medical setting. This was announced in the “Proposal Request for Research on Classification of National Essential Drugs and Measures for Stable Supply” announced by the Ministry of Food and Drug Safety on the 23rd. The MFDS designates and manages essential medicines that need a stable supply because they are necessary for medical use, such as disease control and radiation disaster prevention, Efforts have been made to ensure a stable supply of essential medicines, including improving the designation criteria, introducing a reevaluation system, providing administrative support for expedited approval, and revising laws. The study plans to review cases from other countries to develop measures to improve the current system. Following the recruitment of researchers, KRW 50 million will be invested over a period of 6 months to conduct the following: ▲survey and compare the operation and utilization of essential medicine systems in major countries; ▲analyze the current status of national essential medicine operations and explore directions for improvement; and ▲analyze the current status of utilization and explore directions for improvement to ensure the stable supply of national essential medicines. First, the study will examine the purpose of essential medicine management in other countries, classification methods (product characteristics, uses, etc.), selection criteria and procedures, and consultation processes. It will also investigate the current status of policy support and preferential measures for stable supply. In addition, the study will derive key considerations for designating national essential medicines based on the characteristics of each item and prepare proposals for improving the standards for designating national essential medicines. The study will also review the classification methods for national essential medicines by use, referencing the WHO Model List of Essential Medicines, to revise the list. The list will be revised based on a comprehensive review of the necessity of each item within the category when designating or reevaluating national essential medicines. In addition, the purpose of the national essential medicines system and the need to distinguish it from similar systems will be considered, and the scope of designation and exclusion of national essential medicines be reviewed. This study will also establish a reorganization and operational plan for the Stable Supply Council and Subcouncil to facilitate discussions on the designation and stable supply of national essential medicines. The study will identify government policy tools and collaboration requirements with relevant ministries and agencies to ensure that stable supply policies decided through the council are implemented, and will review measures to strengthen human and material infrastructure for the stable supply of essential medicines. The MFDS stated, “The supply of essential medicines continues to be an ongoing issue, and we expect the government to play a stronger role in improving the national essential medicines system and ensuring a stable supply in response to environmental changes in various fields.”
- Company
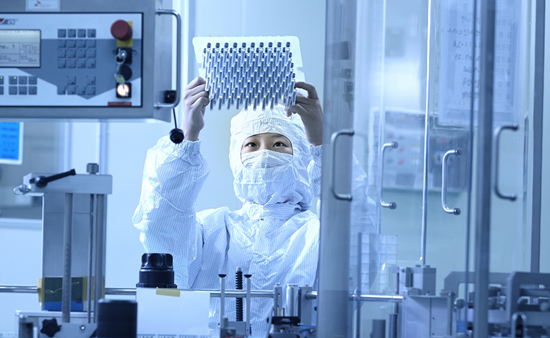
- SK Bioscience wins patent nullity trial against Moderna's
- by Kim, Jin-Gu Apr 24, 2025 06:01am
- SK Bioscience researcher conducting an experiment related to mRNA (photo by SK Bioscience) SK Bioscience reported on April 23 that it won patent nullity against Moderna's mRNA manufacturing technology patent. Moderna’s use patent is the only mRNA manufacturing technology patent registered in Korea. Korea's Intellectual Property Trial and Appeal Board recently issued a decision in favor of SK Bioscience in an invalidation trial against Moderna’s patent titled 'Modified nucleosides, nucleotides, and nucleic acids and their uses.' Moderna did not file a petition to cancel that decision within the allotted time. As a result, the first-instance ruling has been finallized, giving SK Bioscience’s victory. Moderna’s patent has served as core technology for mRNA vaccine production. In South Korea, Moderna’s use patent is the sole registered patent covering mRNA manufacturing methods. SK Bioscience filed the invalidation trial against that patent in 2023. The company determined that the patent is granting undue priority and excessive exclusivity, thereby hampering mRNA vaccine technology development, and brought the suit. After about two years of proceedings, the Korea's Intellectual Property Trial and Appeal Board found that the patent’s appropriatness, priority claim, and inventive step were all invalid. This patent will apply to SK Bioscience’s Japanese encephalitis vaccine candidate 'GBP560' and others in development. With this ruling, SK Bioscience expects its global clinical trials of GBP560 to gain momentum. SK Bioscience began global Phase 1/2 clinical studies of GBP560 in February. These trials are evaluating immunogenicity and safety following GBP560 administration in 402 healthy adults in Australia and New Zealand. The company anticipates interim results will be available next year. SK Bioscience's mRNA vaccine development began in 2022 under an agreement to receive USD 40 million in initial R&D funding from CEPI (Coalition for Epidemic Preparedness Innovations). Once it enters late-stage development after completing Phase 1/2 trials, CEPI will provide up to an additional USD 100 million to SK Bioscience. SK Bioscience spokesperson stated, "We secured a competitive edge in global mRNA vaccine development through this patent case," and added, "While many global firms are still undergoing patent disputes with Moderna, SK Bioscience has led the way in dismantling patent barriers and advancing its proprietary technology." "By reducing patent risk for domestic mRNA developers, we expect to contribute significantly to establishing vaccine sovereignty," the spokesperson emphasized. "SK Bioscience plans to establish an mRNA vaccine platform capable of addressing a broad range of diseases beyond pandemic response and to build new pipelines to achieve global competitiveness," he added. According to the global market research firm Nova One Advisor, the mRNA therapeutics market is anticipated to grow at a 17% compound annual rate, reaching USD 58.9 billion (approximately KRW 84 trillion) by 2033.
- Policy
- Psychotropic drug etomidate will be discontinued in KOR
- by Lee, Hye-Kyung Apr 24, 2025 06:01am
- The domestic supply of etomidate, a psychotropic drug scheduled to be newly designated this year, is expected to be discontinued. According to the Ministry of Food and Drug Safety's list of discontinued and shortage drugs, B. Braun Korea reported on the 21st that it would discontinue the supply of ‘Etomidate-lipuro Injection.’ B. Braun Korea explained, “The drug is scheduled to be designated as a psychotropic substance, which will result in the termination of the current sales contract with the domestic distributor by the end of this year. At this time, the possibility of renewing the contract or entering into a new contract for the drug is unclear, with the future import and supply of the drug plan also undecided.” The MFDS conducted a public consultation until the 10th regarding the “Revision of the Enforcement Decree of the Act on the Control of Narcotics” on whether to newly designate etomidate as a psychotropic drug. Etomidate has been illegally administered or misused in some medical institutions, and the MFDS announced that it will proactively designate it as a narcotic and actively manage it to ensure its safe use in Korea. B. Braun Korea explained, “The medication in question is an injection containing etomidate, and there are no other products with the same ingredient. However, medications with similar efficacy and effects, such as propofol, ketamine, and midazolam, are currently in circulation in the country.”
- Company
- Tuberculosis drug Dovprela lands in Big 5 hospitals in Korea
- by Eo, Yun-Ho Apr 24, 2025 06:01am
- ‘Dovprela,’ the first new drug introduced in the field of tuberculosis in half a century, can now be prescribed at general hospitals in Korea. According to industry sources, Viatris Korea's multidrug-resistant tuberculosis treatment Dovprela (pretomanid) passed the Drug Committees (DCs) of the Big 5 tertiary hospitals in Korea, including Samsung Medical Center, Seoul National University Hospital, Seoul St. Mary's Hospital, and Asan Medical Center. Dovprela, which was first approved in September 2019 in the US and in October 2021 in Korea, is indicated in combination with bedaquiline and linezolid to treat adult patients with extensively drug-resistant (XDR), or treatment-intolerant or nonresponsive multidrug-resistant (MDR) pulmonary tuberculosis (TB). It was listed for reimbursement in January 2023. Pretomanid is the first new drug introduced in the field in 50 years. The field of TB has been neglected by front-line pharmaceutical companies due to its lack of economic feasibility. In fact, Viatris developed the drug in collaboration with a non-profit organization, ‘TB Alliance,’ rather than a general pharmaceutical company. Multi-drug resistant tuberculosis is a type of tuberculosis that cannot be treated with two or more TB treatments including isoniazid and rifampicin, the two most effective anti-TB treatments due to intolerance. Its cause can be divided into primary resistance and acquired resistance. Primary resistance develops when a patient is infected with drug-resistant MTB or during the course of treatment due to arbitrary discontinuation of therapy or irregular administration, etc. Treatment success rate of multi-drug resistant tuberculosis is around 50%, it has low treatment efficiency, and second-line drugs used for its treatment bring more side effects than first-line drugs. Moreover, due to its longer treatment period of 18 to 24 months, the cost burden is high and may even require surgical operations to remove lesions. Also, the seven-drug combination therapy that includes bedaquiline (Bdq) which is used as the current standard treatment for multidrug-resistant tuberculosis, is not well used in Korea due to its high drug resistance rate and long treatment period of 9 to 12 months. Due to the long period, the 7-drug combination is difficult to manage and has a high failure rate. Meanwhile, Dovprela demonstrated its efficacy through the Phase III Nix-TB trial. Dovprela, in combination with bedaquiline and linezolid (BPaL), demonstrated a 92% effect in patients with treatment-intolerant or nonresponsive multidrug-resistant TB and an 89% effect in patients with extensively drug-resistant TB within 6 months and demonstrated its potential as a new short-term combination therapy in the field. Also, it reduced the treatment period from 18-24 months to 6 months, and almost all patients with treatment-intolerant or nonresponsive multidrug-resistant TB and extensively drug-resistant TB were found to be sputum culture-negative within 16 weeks. As the first ready-to-use combination that consists solely of oral treatments, the BPaL regimen reported a 90% cure rate in patients with extensively drug-resistant tuberculosis when used for 6 months compared to the standard treatment that recommends the use of at least 4 drugs in the initial intensive phase.
- Company
- 1 out of 2 multinational firms saw SG&A expenses ratio↓
- by Son, Hyung Min Apr 24, 2025 06:01am
- It was reported that multinational companies reduced their selling, general, and administrative (SG&A) expenses (hereafter referred to as SG&A expenses). Analysis suggests that the recent medical dispute in South Korea impacted the sales and R&D activities. In contrast, pharmaceutical companies with increased SG&A expenses saw a surge in severance payment ratio due to early retirement plans (ERP). According to the Financial Supervisory Service (FSS) on April 24, SG&A expenses for 30 major multinational pharmaceutical companies’ Korean subsidiaries totaled KRW 1.8373 trillion last year, a 0.8% increase from the year before. Among those 30 companies, 17 increased their SG&A expenses, while 16 saw their expense-to-revenue ratios decline. Selling, general, and administrative (SG&A) expenses of major multinational companies in KOR (unit: KRW 1 million) Lilly Korea’s SG&A expenses amounted to KRW 37.2 billion, down 2% year-on-year (YoY), and its expense to sales ratio declined by 6%. R&D expenses, which include academic research and ongoing trial costs, dropped 25%, from KRW 6.4 billion in 2023 to KRW 4.7 billion last year. As Lilly supplies new drugs for oncology and biologics to tertiary hospitals, medical-government disputes significantly affected Lilly's R&D expenses. MSD Korea cut its SG&A expenses by 11%, from KRW 104.9 billion in 2023 to KRW 93.6 billion. The company had a significant reduction in R&D spending. MSD Korea's research expenses dropped 48% from KRW 9.2 billion to KRW 4.8 billion. Both lower research budgets and workforce reduction likely affected this shift. GSK Korea also reduced its current research expenses by 72%, from KRW 8.9 billion to KRW 2.5 billion, and Novartis Korea, which had the highest SG&A expenses last year, saw a reduction in SG&A expenses from KRW 29.6 billion to KRW 28.0 billion, a 5% decrease. Salaries spending impacted changes in SG&A expenses Changes in salaries, severance payments, and retirement benefits, also affected expense changes in several companies. AstraZeneca Korea's SG&A expenses fell 26% to KRW 107.5 billion. Its expense ratio dropped 5% from that of 2023. The company's base salaries, retirement benefits, severance, and welfare outlays all decreased. AstraZeneca conducted an ERP following the withdrawal of Forxiga from South Korea in 2023. The severance costs amounted to KRW 25.7 billion in 2023 but declined to KRW 0.081 billion last year. The total payroll dropped 14% from KRW 37.1 billion to KRW 31.8 billion. In contrast, Kyowa Kirin Korea's ERP drove SG&A expenses higher. The company recorded a total payroll of KRW 8.2 billion, and severance payouts amounted to KRW 26.1 billion. The payroll declined by 15%, but severance payouts surged by 1,410%. Kyowa Kirin Korea conducted an ERP last year. The company sold its Asia-Pacific unit last year, China operations to Hong Kong's Winhealth Pharma, and regional promotional and distribution arms to DKSH last month. Janssen Korea's SG&A expenses increased due to increased payroll and retirement benefits. The company saw a 13% rise in SG&A expenses from the previous year to KRW 88.0 billion. Its total payroll rose 9% to KRW 27.4 billion, and retirement benefits increased 24%. As the company's KRW 3.8 billion severance cost from 2023 was reflected on the audit report, the SG&A cost surged.
- Company
- AbbVie’s workforce↑ MSD↓ due to business restructuring
- by Son, Hyung Min Apr 24, 2025 06:01am
- Various factors, including the sale of drug rights, early retirement programs (ERP), and the launch of new drugs, have affected the number of employees at Korean subsidiaries of multinational pharmaceutical companies. AbbVie Korea doubled its workforce over 4 years through the Allergan merger. BMS Korea, Merck, and Novo Nordisk Korea saw significant increases in staff upon the launch of their innovative new drugs and business expansion. MSD Korea had the largest number of employees as of last year, but this decreased by 200 in four years due to the sale of Januvia rights and the implementation of ERP. Pfizer Korea, Janssen Korea, AstraZeneca Korea, and Novartis Korea also saw a decrease in the number of employees due to the adoption of ERP. According to an analysis of the audit reports of 30 multinational pharmaceutical companies in Korea disclosed on the Financial Supervisory Service's electronic disclosure system on the 23rd, the total number of employees last year was 7,389, an increase of 68 from 7,321 the previous year. Compared to 7,192 in 2020, this is an increase of 197 in four years. The company with the largest increase in employees compared to 2020 was AbbVie Korea. The number of employees at AbbVie Korea last year was 340, a 17 increase from the previous year. The company's employee count rose significantly from 170 in 2020 to 323 in 2023. AbbVie Korea acquired 100% of the shares of Allergan Korea on February 1, 2023. On April 30 of the same year, it absorbed Allergan Korea, and from the following day, Allergan Korea's performance began to be reflected in AbbVie Korea's results. The merger and acquisition at the headquarters level was carried out in 2019. On June 25, 2019, AbbVie acquired Allergan for USD 63 billion (approximately KRW 73 trillion). Allergan owns the original botulinum toxin product “Botox.” Merck, Novo Nordisk, and BMS Korea saw a significant increase in their number of employees with the launch of innovative new drugs. BMS Korea surpassed 200 employees for the first time last year. The company's workforce reached 209 employees last year, a 24 increase from the previous year. The company has consistently expanded its workforce while supplying immunotherapy drugs such as Opdivo, heart failure treatment Camzyos, anticoagulant Eliquis, and leukemia drug Sprycel in Korea. In addition, BMS Korea signed a joint promotion agreement with Yuhan Corporation last year for the psoriasis treatment of Sotyktu and the ulcerative colitis treatment of Zeposia. As a result, the company established a new Immunology Sales Department and hired additional clinical team members, leading to an increase in the number of employees. The number of employees at Merck Korea increased by 39.4% from 345 in 2020 to 481 last year. This means that 136 new employees were hired over the past four years. Looking at the numbers by year, the number of employees steadily increased from 360 in 2021 to 409 in 2022 and 444 in 2023, reflecting the company's strategy to expand its business in Korea. Merck has achieved remarkable results in various fields, including infertility treatments and anticancer drugs. In April last year, Merck's Pergoveris Inj for ovulation induction was granted reimbursement for infertility. In addition, the company is expanding its business by supplying the non-small cell lung cancer treatment Tepmetko and the bladder cancer treatment Bavencio in Korea. Novo Nordisk also showed a clear upward trend, increasing its number of employees from 169 in 2020 to 291 in 2024, which was a 72 increase. This is believed to be related to the growth of GLP-1 (glucagon-like peptide-1) class obesity and diabetes treatments in the domestic market. Novo Nordisk has launched not only GLP-1 new drugs containing liraglutide, such as Saxenda and Victoza but also diabetes drug Ozempic and obesity drug Wegovy containing semaglutide in the domestic market. Wegovy, which entered the market in the fourth quarter of last year, surpassed KRW 60 billion in sales in just one quarter. Sales right transfers, withdrawal from the Korean market, and ERP lead to layoffs On the other hand, some companies have reduced their workforce due to the impact of sales, withdrawal from the Korean market, and ERP. Last year, MSD Korea had 505 employees, which was a 201 decrease from 2020. The biggest factor affecting this reduction of workforce was the spin-off of Organon. Organon was spun off from Korea MSD in 2021 and officially launched in June of the same year. Organon sells chronic disease treatments such as Propecia for hair loss, Cozaar for hypertension, and Atorvastatin for dyslipidemia, which was previously sold by MSD. MSD Korea has transferred the Januvia family to Chong Kun Dang and reorganized its chronic disease business division. The company transferred the rights for Januvia (sitagliptin), Janumet (sitagliptin and metformin), Janumet XR (sitagliptin and metformin), and other Januvia family products, as well as the diabetes drugs Steglatro and Steglujan to Chong Kun Dang in May 2023. At the same time, it closed down its General Medicine (GM) division. The number of employees at Pfizer Korea decreased by 50 from 454 in 2023 to 404 last year. The honorary retirement benefits paid last year amounted to KRW 5.33526 billion, a 279.9% increase from the previous year's KRW 1.4453 billion. Pfizer carried out global restructuring in 2023 and last year. This was due to a sharp decline in sales of vaccines and treatments such as Comirnaty and Paxlovid following the COVID-19 pandemic. This decision also affected the reduction in staff at the Korean branch. Novartis Korea had 466 employees last year, a decrease of 68 in the past four years. Novartis underwent a large-scale restructuring at the headquarters level in 2022. In response, Novartis Korea reorganized its respiratory division in 2022. Novartis Korea's respiratory treatments include Enerzair, a triple combination asthma treatment, and Atectura, a once-daily fixed-dose combination medication. Xolair, Novartis Korea's best-selling asthma treatment, was not included in the restructuring as it was an immune disease division product. In addition, Novartis Korea's generic drug division, Sandoz, was spun off and then withdrawn from the Korean market in 2023. In the same year, Novartis Korea began restructuring its portfolio by implementing ERP for its ophthalmology division. AstraZeneca Korea is one of the companies that has experienced significant fluctuations in the number of employees. The company's workforce increased by 18 employees from 393 in 2020 to 411 last year. However, compared to 439 employees in 2023, last year's figure represents a decrease of 28 employees. The increase in AstraZeneca Korea's workforce was attributed to its business expansion. AstraZeneca acquired Alexion, a company specializing in the development of rare disease treatments, in 2020. Alexion holds rare disease drugs Soliris and Ulotrimis, which are used for conditions such as paroxysmal nocturnal hemoglobinopathy and severe myasthenia gravis. AstraZeneca Korea began domestic sales of the drugs in February 2023, leading to an increase in the number of employees in the rare disease division. Meanwhile, the primary reason for the decrease in the number of employees at AstraZeneca Korea last year was the withdrawal of the SGLT-2 inhibitor-based diabetes treatment drug Forxiga from the Korean market. The company implemented an ERP for the CVRM (Cardio Vascular Renal Metabolism) division, which previously housed the Forxiga sales department.