- LOGIN
- MemberShip
- 2026-03-10 00:56:55
- Policy
- Fast-track listing of "high-priced new drugs" raises concerns
- by Jung, Heung-Jun Feb 10, 2026 08:13am
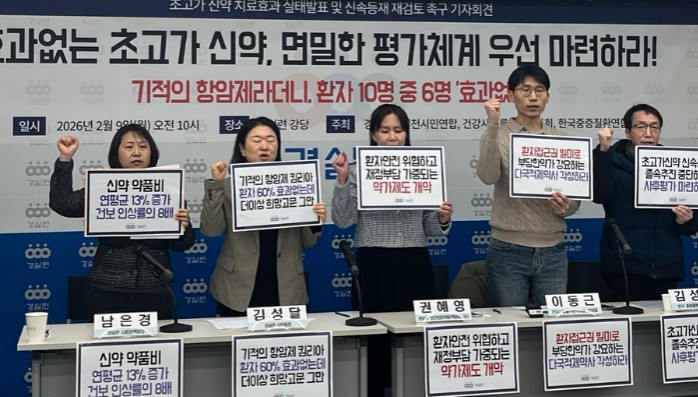
- The Citizens' Coalition for Economic Justice (CCEJ) has urged the government to reconsider the fast-track reimbursement policy for rare disease treatments.They are citing concerns that health insurance finances could be wasted on high-priced drugs with unverified efficacy.On the morning of the 9th, the CCEJ, joined by the Korean Pharmacists Associations and the Korea Severe Disease Association raised concerns about the government policy aimed at increasing treatment accessibility for rare diseases. On the 9th, the Citizens' Coalition for Economic Justice, joined by the Korean Pharmacists Associations and the Korea Severe Disease Association held a press conference to demand an immediate halt to the fast-track initiative for ultra-expensive new drugs. The groups argued that the government should prioritize establishing post-marketing evaluation measures over the hasty expansion of health insurance coverage for new drugs.These associations said, "The government announced a fast-track policy to reduce the reimbursement listing period from 240 days to 100 days to improve access," adding, "While the previous process required 150 days to review clinical utility and cost-effectiveness, the new plan bypasses these steps, completing the establishment of benefit criteria within a single month."They pointed out that this effectively eliminates the need to verify a drug’s clinical value. They also condemned the plan to reference the average listed prices of eight major countries (A8) to determine drug costs."While prices were previously negotiated over 60 days based on a drug's value, the reform aims to decide prices within a month based on overseas list prices, which are often inflated compared to actual transaction costs," they stated, "This is likely to reflect the high prices desired by pharmaceutical companies." Performance Evaluation Results (HIRA) for High-priced Medicines. 1. Evrysdi POS (risdiplam), 2. Spinraza Injection(nusinersen), 3. Luxturna injection (voretigene neparvovec), 4. Kymriah Inj (tisagenlecleucel), 5. Zolgensma injection (onasemnogene abeparvovec).Furthermore, they also raised concerns about waste of health insurance funds based on the results of survey on the status of the effectiveness of high-priced new drugs.The organizations based their criticism on HIRA's performance evaluation data for the 5 ingredients of 8 high-priced drugs under the performance-based Risk Sharing Arrangement (RSA).According to data provided by HIRA to Representative Seo Young-seok's office, even Kymriah, so-called a 'miracle' treatment, showed that 59.1% of treated patients did not achieve the expected therapeutic effect. The organizations estimated that this led to approximately KRW 76.6 billion in unnecessary health insurance drug expenditures.Additionally, Spinraza (nusinersen) and Luxturna (voretigene neparvovec) also recorded a 50% failure rate in meeting performance evaluation standards."Over half of the patients who were treated with Spinraza and Luxturna, despite being subject to a 'prior approval system' that audits patient eligibility before administration," and added, "Based on the results from the French health authorities evaluating ultra-expensive drugs on the Korean market, 54% of the list showed either no or only marginal efficacy improvements compared to existing therapies."They estimated that if 53 of the 77 rare disease drugs currently awaiting reimbursement are listed under the new 100-day 'fast-track' rule, it would require an additional KRW 1.5 trillion in insurance funding. They criticized the government for essentially 'blinding' the evaluation system by skipping clinical and economic feasibility checks and relying on the 'price bubble' of major foreign (A8) listed prices.To address these issues, the organizations demanded ▲full public disclosure of all new drug efficacy evaluations ▲establishment of a specified post-marketing evaluation measure ▲establishment of financial management for new drugs ▲establishment of a social discussion body.They stated, "Policies that subject people to potential clinical test subjects with unwarranted efficacy must be halted. We urge the government to secure justification and safety of the policy through social discussions, rather than a closed administrative action. The government must now establish a transparent and fair social discussion body."
- Policy
- MOHW ‘Limited impact’ vs Industry ‘₩3 trillion loss’
- by Lee, Jeong-Hwan Feb 09, 2026 07:33am
- Calls are growing for the Ministry of Health and Welfare (MOHW) to begin public–private consultations based on the results of its internal analysis of the impact of generic drug price cuts.The ministry is said to have concluded, based on its own quantitative analysis of the impact on each pharmaceutical company when drug price cuts are implemented, that the industry’s estimated losses of up to KRW 3 trillion resulting from the price cuts are inaccurate. However, the Ministry has not publicly disclosed the simulation results, drawing criticism from the pharmaceutical industry.The pharmaceutical industry maintains that the government should transparently disclose the results and analytical criteria of its own drug price reduction simulations and begin discussions on policy revisions directly with the pharmaceutical industry, the primary stakeholders. Attention is focused on whether the MOHW will accept this request.According to government and industry sources on the 6th, the MOHW began internal simulations to assess the impact of price reductions for already-listed generic drugs, a key element of the drug pricing reform plan announced on November 28 last year.Sources say the Ministry's simulation results show a significantly lower figure than the pharmaceutical industry's claim of ‘up to KRW 3 trillion in sales losses’.The Ministry of Health and Welfare's own analysis indicates that the projected revenue loss from drug price reductions per pharmaceutical company, calculated using the current 53.55% generic drug reimbursement rate and the discount/preferential rates to be applied during the drug pricing system reform (based on factors like each company's R&D expenditure relative to sales), falls significantly short of the industry's own estimates.The pharmaceutical industry fears that, based on these results, the MOHW will continue its stance that it can push through the previously announced reform plan with minimal changes, relying on its own simulation findings.Consequently, multiple pharmaceutical companies are raising the need for public-private discussions regarding the ministry’s simulation results.The argument is that implementing such a major drug price overhaul, the first in approximately 14 years since the 2012 blanket price reduction, without proper consultation procedures, finalizing and enforcing it just three months after announcement, constitutes excessive infringement on the industry’s right to express its views.In particular, industry stakeholders dispute the ministry’s claim that companies certified as innovative pharmaceutical companies or those with high R&D-to-sales ratios would be exempt from the negative impact of price cuts.The argument is that after the price reform, companies that have invested heavily to obtain innovative-company certification or to develop and manufacture high-quality generics may see little to no preferential treatment compared with those with low investment and those that merely contract manufacturing generics. In the worst cases, there could even be a reversal where profits decrease compared to non-investing companies.With the positions of the MOHW and pharmaceutical companies sharply at odds over the same reform proposal, attention is turning to whether public–private consultations can take place ahead of the plan’s submission and deliberation at the Health Insurance Policy Deliberation Committee later this month.A pricing manager at domestic pharmaceutical company A stated, “The Ministry of Health and Welfare validated its drug price reform plan based on its own simulation of pharmaceutical companies' sales losses from price cuts, yet it hasn't actually disclosed the simulation criteria or results. Only by initiating mutual discussions with pharmaceutical companies centered on the government’s analysis results would we be able to move closer to a reform that minimizes conflict.”A pricing manager from another pharmaceutical company, B, also pointed out, “The Ministry should fully incorporate the specific positions of direct stakeholders like pharmaceutical companies regarding the problems with the drug price reduction system, but so far, the Ministry hasn't been taking an active stance toward gathering opinions. The government and the industry may be using entirely different indicators to calculate the impact of price cuts. Without sharing the raw data, meaningful consultation is impossible.”He added, “Even R&D-focused or innovative pharmaceutical companies report that, based on their own simulations, the ministry’s proposed price cuts would not provide real preferential benefits and could even push operating profits into deficit. There is serious concern that this reform plan, which could undermine the will to contribute to new drug development and solving supply instability issues, might be finalized and enforced without modification.”
- Policy
- AbbVie’s Parkinson’s drug receives orphan drug designation in Korea
- by Lee, Tak-Sun Feb 09, 2026 07:32am
- A new Parkinson's disease treatment drug approved by the U.S. Food and Drug Administration (FDA) has been designated as an orphan drug in Korea.As orphan drug designation enables expedited review, potentially shortening the approval timeline, expectations are rising for the drug’s earlier commercialization.According to the Ministry of Food and Drug Safety (MFDS), the foscarbidopa/foslevodopa injection was officially designated as an orphan drug on February 3.The drug is indicated for adults with advanced Parkinson’s disease who experience severe motor fluctuations that are not adequately controlled with existing Parkinson’s therapies.The foscarbidopa/foslevodopa injection mentioned by the MFDS was Vyalev, AbbVie’s Parkinson’s drug approved by the FDA in 2024.Vyalev is the first and only 24-hour levodopa-based continuous subcutaneous infusion for treating motor fluctuations in adults with advanced Parkinson's disease.Patients with advanced Parkinson’s disease often struggle to manage motor fluctuations. Vyalev offers the benefit of continuous symptom control through continuous 24-hour drug delivery.In particular, the therapy is expected to reduce the number of times when the effect of oral medications wears off, and movement becomes difficult, thereby offering a new treatment option that can meaningfully improve quality of life for patients with advanced Parkinson’s disease.In October last year, Korea Parkinson’s Hope Alliance held a press conference urging the introduction of Vyalev in Korea. Although Vyalev has already been launched in 35 countries, including the United States, Europe, and Japan, it has not yet received formal approval in Korea.Once designated as an orphan drug, a product becomes eligible for conditional approval, reduced regulatory fees, exemptions from certain bridging data requirements, and priority review, all of which streamline the regulatory process and accelerate approval. Therefore, attention is now focused on whether this orphan drug designation will accelerate Vyalev’s introduction into the domestic market.Recently, the MFDS has relaxed orphan drug designation requirements, lowering the regulatory threshold. Previously, applicants were required to submit data demonstrating improved efficacy over alternative therapies, but under the revised criteria, such data are no longer mandatory for orphan drug designation.
- Policy
- HIRA to reinforce staff for post-listing evaluation
- by Jung, Heung-Jun Feb 06, 2026 06:43am
- The Health Insurance Review and Assessment Service (HIRA) has begun reinforcing post-listing evaluation by expanding personnel and restructuring its organization in preparation for shortened listing timelines for rare disease drugs.The existing Pharmaceutical Performance Assessment Department has been reorganized into the Rare & Severe Disease Pharmaceutical Performance Assessment Department within the Health Insurance Innovation Center, accompanied by staffing reinforcements.As evaluation procedures must be streamlined to shorten listing periods, post-listing assessment of clinical outcomes will be intensified.On the afternoon of the 4th, HIRA President Jung-gu Kang explained the plan to shorten the listing period for rare disease treatments, included in the proposed drug pricing reform plan, during a briefing with press corps reporters.The drug pricing reform plan reported to the Health Insurance Policy Deliberation Committee (HIPDC) in January includes a policy to enable fast-track reimbursement listing of rare disease drugs within 100 days.Kang stated, “We will simplify reimbursement appropriateness evaluation and negotiation procedures to shorten listing timelines and improve patient access. Conversely, to strengthen post-listing evaluation and ensure internal scalability, we have reorganized the existing Pharmaceutical Performance Assessment Department into the Rare & Severe Disease Pharmaceutical Performance Assessment Department within the Health Insurance Innovation Center and increased staffing.”In the first half of this year, HIRA also plans to commission research projects aimed at establishing cost-effectiveness evaluation criteria for new drugs.Kang said, “Through these research projects, we will develop an ICER threshold and adjustment framework suited to the Korean context, thereby building a rational and sustainable cost-effectiveness evaluation system.”Furthermore, to strengthen post-market evaluation for new drugs with unclear clinical evidence, plans are underway to utilize Real-World Data (RWD) and Real-World Evidence (RWE).Guidelines were developed based on the results of a research project conducted from March to November last year. Currently, registries for 12 drugs are being established to conduct performance assessments.The drugs under evaluation include Kymriah, Zolgensma, Spinraza, Evrysdi dry syrup, Luxturna, Qarziba, Bylvay capsules, Livmarli oral solution, Ilaris, Pemazyre, Zepzelca, and Isturisa film-coated tablets.Kang stated, “We revised detailed evaluation criteria to establish a solid foundation that enables outcome assessment using RWD. We will enhance the utilization of RWE generation guidelines, systematically manage registry quality to continuously verify clinical value, and strive to ensure patient safety.”Advancing health insurance payment reform… reviewing introducing a parallel fee scheduleBeyond drug-related issues, HIRA also outlined plans to develop a roadmap for reforming the national health insurance payment system. HIRA is reviewing a parallel payment model that combines fee-for-service and diagnosis-related group (DRG) payment system.For example, fee-for-service reimbursement would be maintained for physicians’ specialized surgical procedures and interventions, while hospital system usage fees, such as hospitalization charges or examination fees, would be compensated under a bundled payment system by DRG.HIRA also plans to further refine the Clinical Practice Evaluation Panel (CPEP) system, which precisely measures physician effort and equipment costs associated with individual medical services. The goal is to reassess and appropriately revalue services that have been historically undervalued.Kang explained, “Based on research recommendations, we are reviewing relative value payment reforms, including further refinement of CPEP to reform the current fee-for-service system. We are also considering the introduction of parallel payment models in relation to bundled payments.”He added, “We will shorten the cycle of the relative value score adjustment structure, which is a national policy task, and ultimately transition to a continuous adjustment system. This will help break away from the structure where profits increase only by performing many tests, and instead support a more realistic and sustainable reimbursement system.”
- Policy
- HK Inno.N enters Prolia biosimilar market
- by Lee, Tak-Sun Feb 06, 2026 06:43am
- HK Inno.N has joined the biosimilar market for the osteoporosis treatment Prolia (denosumab).It is the third company to obtain regulatory approval for a Prolia biosimilar, following Celltrion and Samsung Bioepis. Competition in the approximately KRW 170 billion market is expected to intensify.Korea’s Ministry of Food and Drug Safety approved HK Inno.N’s Izambia Prefilled Syringe (denosumab) on the 4th.Izambia is a biosimilar with the same efficacy and effects as the original drug, Prolia Prefilled Syringe, which contains the same active ingredient. It is indicated for: ▲ Treatment of osteoporosis in postmenopausal women ▲ Treatment to increase bone mineral density in men with osteoporosis ▲ Treatment of glucocorticoid-induced osteoporosis ▲ Treatment of bone loss in non-metastatic prostate cancer patients receiving androgen deprivation therapy ▲ Treatment of bone loss in female breast cancer patients receiving adjuvant aromatase inhibitor therapy.Izambia was licensed from Spain’s mAbxience. In January 2023, HK inno.N signed an exclusive domestic licensing agreement with mAbxience for denosumab biosimilars. Under the agreement, HK inno.N secured exclusive supply rights for two denosumab biosimilars, as well as domestic regulatory approval and commercialization rights.Denosumab is an antibody therapy that targets the ‘RANKL’ protein, which is critical for the survival and function of osteoclasts, thereby exerting potent inhibition of bone resorption. The original drugs are Amgen's osteoporosis treatment ‘Prolia’ and ‘Xgeva’, used for preventing skeletal-related events in patients with bone metastases and treating giant cell tumor of bone. Both products were launched in 2016.On the same day, HK inno.N also received approval for Denbrayce Inj, a biosimilar to Xgeva.Amgen’s ProliaProlia, which recorded annual sales of approximately KRW 174.9 billion in 2024 (IQVIA data), began facing biosimilar competition after its substance patent expired in March last year. Celltrion’s Stoboclo was the first biosimilar to launch, followed by Samsung Bioepis’ Obodence last year.Stoboclo is co-marketed by Daewoong Pharmaceutical, while Obodence is co-marketed by Hanmi Pharmaceutical. Given that the original Prolia is co-marketed in Korea by Chong Kun Dang and Amgen, the denosumab market has effectively become a battleground for major domestic pharmaceutical companies.With HK inno.N now entering the market, competition is expected to further intensify. The newly approved denosumab biosimilars from HK inno.N are expected to be launched within the first half of the year, following completion of reimbursement pricing procedures.
- Policy
- Will the NA pass the 'mandatory INN prescription' bill?
- by Lee, Jeong-Hwan Feb 04, 2026 06:51am
- While the simplified post-notification system for substitution drugs through the government's electronic network was implemented on February 2, the pharmaceutical industry is increasingly focusing on the "limited International Nonproprietary Names (INN) prescription" bills currently pending in the National Assembly.Members of the ruling party on the Health and Welfare Committee have expressed a consensus on the need to accelerate the review of these bills, noting that the Lee Jae Myung administration has chosen mandatory INN prescription for national essential medicines as a national task to resolve supply instabilities.As of February 3, three bills related to limited INN prescription, introduced by Rep. Kim Yoon and Rep. Jang Jong-tae of the Democratic Party, are pending in the National Assembly.Rep. Kim Yoon's Pharmaceutical Affairs Act Bill proposes a legal definition for supply-unstable drugs and allows the Minister of Health and Welfare to recommend the use of INN for national essential and supply-unstable drugs.This method is considered less coercive as it does not mandate health professionals to use INN prescription during patient care and prescription.Rep. Jang Jong-tae's Medical Service Act & Pharmaceutical Affairs Act Bill requires the MOHW to designate supply-unstable drugs after deliberation by a Supply Management Committee. It mandates physicians to use INN instead of brand names when prescribing these designated drugs.Notably, Rep. Jang's proposal is considered highly coercive because it includes a penalty of up to one year in prison or a fine of up to KRW 10 million for physicians who violate the INN mandate.Some ruling party members on the Health and Welfare Committee state that if a legislative subcommittee is held this month, these bills should be officially adopted for review. They argue there is no reason to delay, especially given President Lee's recent criticisms regarding the slow pace of legislation.Rep. Kim's bill has been pending for over a year since its introduction in December 2024.The pharmaceutical industry is showing significant attention as the MOHW and the Health Insurance Review and Assessment Service (HIRA) began the implementation of the simplified post-notification system for substitution drugs, formulations, and dosages on February 2.An official from the Health and Welfare Committee stated, "The ruling and opposition party mangement groups are currently coordinating the schedule for the February legislative subcommittee," and added, "If the schedule is confirmed, there is a high possibility that the INN prescription bills will be placed on the agenda, as they are drawing significant attention from both the proposed offices and the committee members."
- Policy
- Merck’s mirdametinib drug receives GIFT designation
- by Lee, Tak-Sun Feb 04, 2026 06:51am
- Gomekli (mirdametinib) was approved by the US FDA in February last yearMerck’s neurofibromatosis treatment candidate mirdametinib has been designated for the Ministry of Food and Drug Safety’s (MFDS) expedited review support program, GIFT (Global Innovative products on Fast Track).As a result, the drug’s entry into the Korean market is expected to accelerate.According to the MFDS, mirdametinib was designated as a GIFT product on the 20th of last month.GIFT is an expedited review program launched in September 2022 to support rapid product development and provide patients with faster access to new treatment options.The program targets innovative medicines, including those for life-threatening diseases, rare diseases with no existing treatment alternatives, and new drugs developed by certified innovative pharmaceutical companies.The MFDS designates GIFT products based on a comprehensive evaluation of factors such as innovative therapeutic effects, contribution to addressing public health needs, and the developer’s efforts.Once designated, the review period is reduced by at least 25% (from 120 working days to 90 working days).The program also applies rolling reviews, under which submitted data are reviewed on an ongoing basis, and provides close communication between regulators and developers through product briefings and supplementary meetings. In addition, regulatory consulting and other support measures are offered to facilitate rapid commercialization.Mirdametinib is Korea’s 64th GIFT product. The proposed indication submitted to the MFDS is for the treatment of ‘pediatric and adult patients aged 2 years and older with neurofibromatosis type 1 (NF1) who have symptomatic, inoperable plexiform neurofibromas.’Mirdametinib is a selective inhibitor of mitogen-activated protein kinase kinases 1 and 2 (MEK1/2). It exerts antitumor activity by blocking MEK activity, thereby inhibiting the phosphorylation of Extracellular-regulated kinase 1 and 2 (ERK1 and ERK2) within the Mitogen-activated protein (MAP) pathway.It received Fast Track designation from the US FDA on February 11 last year and was approved by the EMA on July 17 last year. In Korea, it was designated as an orphan drug on December 11 last year.Mirdametinib was originally developed by the U.S. biotech company SpringWorks Therapeutics. In April 2023, SpringWorks was acquired by Germany-based Merck for USD 3.9 billion, giving Merck global commercial rights to the drug.Once launched, mirdametinib is expected to compete with the existing neurofibromatosis therapy Koselugo (selumetinib, AstraZeneca).Koselugo, which is also indicated for neurofibromatosis type 1, has been reimbursed by Korea’s national health insurance for patients aged 3 years and older since January 2024.Neurofibromatosis is a type of neurocutaneous syndrome characterized by abnormalities affecting both the skin and the central nervous system. Among its various subtypes, neurofibromatosis type 1 is the most common. Depending on the location of the neurofibromas, patients may exhibit brain tumor symptoms, and spinal involvement can lead to scoliosis. As of 2024, there are 6,490 known patients in South Korea.With recent increases in cases of reduced reimbursement for Koselugo, calls for improving reimbursement criteria are growing among neurofibromatosis patients and medical professionals.
- Policy
- Novartis withdraws all statin agents from the Korean mkt
- by Lee, Tak-Sun Feb 03, 2026 10:32pm
- Product photo of LescolNovartis is withdrawing all its statin agents used to treat hyperlipidemia from the Korean pharmaceutical market.Analysis suggests that the product's competitiveness has weakened due to other statin agents.According to the Ministry of Food and Drug Safety (MFDS) on the 2nd, Novartis Korea reported discontinuing supply of 'Lescol XL Tab (fluvastatin sodium),' the company's only statin-containing drug.Novartis stated, "In accordance with our global strategy and supply planning, we are discontinuing the supply of Lescol XL extended-release Tablet."The supply discontinuation date is set for July 31. Novartis noted, "Following the discontinuation of supply, please consider substituting with other statin-based products of the same mechanism of action (e.g., rosuvastatin, atorvastatin, simvastatin, pravastatin, etc.)."Lescol XL Extended-Release Tablet is currently the only statin product from Novartis that remains approved.Novartis entered the statin market in Korea in 1994, after obtaining MFDS approval for Lescol capsule. However, the product failed to achieve high performance as it lost out in competition with other statin products.Consequently, five of the six approved fluvastatin items were removed from the approval list in 2022 and 2023 due to withdrawals.Lescol XL was the only remaining product. However, following the latest report of supply discontinuation, fluvastatin will be completely withdrawn from the Korean market. There are currently no separate generic items available.Lescol XL Tab is indicated for ▲reduction of risk for cardiovascular disease, ▲hyperlipidemia ▲an adjunct to diet to reduce elevated total cholesterol, LDL-cholesterol, apo-B protein, and triglyceride levels and to increase HDL-cholesterol in pediatric and adolescent patients (boys: aged 9 to 16; girls: aged 10 to 16 and post-menarche) with heterozygous familial hypercholesterolemia who do not respond adequately to dietary therapy.Based on 2024 UBIST data, outpatient prescription amount totaled KRW 2.8 billion, a 23.7% decrease from the previous year. The sales volume is considered small when compared to Viatris' Lipitor (atorvastatin calcium trihydrate), a statin agent, which recorded KRW 188.6 billion in prescription sales during the same period.The underperformance is considered the most significant factor in this withdrawal from the Korean market.
- Policy
- Pharma, preparing for the future…generic launch in 2030s
- by Lee, Tak-Sun Feb 03, 2026 06:24am
- Product photos of Tagrisso (left) and K-CAB (right).Are they already preparing for the future? The Korean pharmaceutical industry is preparing for generics that would be launched five years later. They are also fiercely competing to secure priority marketing authorization by filing patent applications and seeking approvals.According to the Ministry of Food and Drug Safety (MFDS), 'Otinib tablet (Chong Kun Dang),' a generic version of the non-small cell lung cancer treatment Tagrisso (osimertinib), was approved on the 27th and also secured the priority marketing authorization. When assigned a priority marketing authorization, the drug receives an exclusive sales period of 9 months, during which the sale of generics containing the same active ingredient is banned.However, the effective date of the priority marketing authorization is not approaching soon. It is set to begin on December 28, 2023, and terminate on September 27, 2034. Approximately 8 years remain until the product launch. This is because the Tagrisso patent is set to expire on the specified date.Generic versions of K-CAB (tegoprazan), a P-CAB for gastroesophageal reflux disease (GERD), are increasingly receiving approvals. Yet, the priority marketing authorization is scheduled to take effect after August 26, 2031.Until now, pharmaceutical companies that received K-CAB generic approvals include GC Cross, Withus Pharm, Genuonesciences, Korea Drug, Ildong Pharmaceutical, KyungDong Pharm, and Hutecs Korea.As K-CAB is a mega-blockbuster item generating over KRW 200 billion in annual sales, numerous companies are competing for approvals to gain pre-occupancy in the generic market.Generics to Daiichi Sankyo's neuropathic pain treatment Taleaje (mirogabalin besilate) can be launched on or after 2031.Five pharmaceutical companies have applied for approval of their products containing mirogabalin besilate. Several companies have started patent challenges, excluding substance patents. Huons, Daewoong Pharm, Dong-A ST, JW Pharmaceutical, KyungDong Pharmaceutical, and Samjin Pharm.Five pharmaceutical companies that successfully challenged patents would be leading candidates to obtain priority marketing authorization. Despite this advantage, more than 5 years remain until the launch of generics, as the patent on the active ingredient is set to expire on June 4, 2031.Taleaje is still a non-reimbursed drug, and its sales cannot be estimated yet. Despite this circumstance, Korean generic companies have anticipated the bright future of the Taleaje market and have entered the race to secure a generic position.
- Policy
- Korea’s Innovative Pharmaceutical Company certification overhaul
- by Lee, Jeong-Hwan Feb 03, 2026 06:24am
- Director Kang-seop LimAttention is focused on how much the domestic pharmaceutical industry's request for rationalization of the ‘one-strike-out’ rebate regulation will be reflected in the reform plan for the Korea Innovative Pharmaceutical Company certification system, for which a legislative notice is being prepared by the Ministry of Health and Welfare within February.The MOHW has gathered extensive industry feedback on the current rule mandating the immediate revocation of innovative certification for companies found guilty of illegal rebates. Based on this input, the ministry plans to partially modernize regulations that could excessively hinder innovation in the pharmaceutical industry.However, regarding the previously discussed proposal to shift from immediate revocation to a points-based penalty system for rebate violations, the MOHW said it remains cautious and has not yet reached a decision.On the 1st, Director Kang-seop Lim of the Pharmaceutical and Bio-Industry Division met with the Ministry of Health and Welfare's press corps and explained, “We will announce the legislative notice for the enforcement decrees, enforcement rules, and notices related to innovative pharmaceutical companies by February at the latest.”The overhaul of the Korea Innovative Pharmaceutical Company certification system has emerged as a key issue for the industry, as it will operate in line with the drug pricing reform scheduled for implementation this year.Under the proposed drug pricing reform, price premiums would be applied depending on whether a company is certified as an innovative pharmaceutical company and the proportion of R&D investment in new drugs within such companies.Regarding the industry’s primary demand of converting the immediate revocation of innovative certification for rebate violations to a points-based system, Lim said, “This is still under discussion, and no decision has been made.”However, Lim explained that the ministry is preparing the reform plan in full consideration of the industry's persistent demand that the current penalty, where innovative certification is immediately revoked upon confirmation of a rebate incident, is excessively harsh for pharmaceutical companies dedicated to innovation, including new drug development.As the importance of the certification system has grown significantly with the upcoming drug pricing system reform, Lim explained that the ministry is particularly examining the feasibility of introducing several of the improvement measures requested by pharmaceutical companies.Overall, the MOHW is expected to pursue an administrative approach that maintains a certain level of penalties for unfair pharmaceutical trade resulting from illegal rebates, while improving regulations that excessively revoke or withdraw innovative certification based on overly stringent standards.According to industry sources, discussions are underway on rationalizing elements such as the period of application for penalties imposed on companies involved in rebate violations within the legislative and administrative notice.Lim said, “Pharmaceutical companies have repeatedly requested that the criteria for revoking innovative certification due to rebate violations be made more reasonable than they are now. We are internally reviewing measures that can both partially accommodate industry demands while continuing to regulate illegal rebates.”He added, “The decision on whether to adopt a points-based system is still under discussion. Currently, a rebate violation immediately renders a company ineligible as an innovative pharmaceutical company, leading to automatic revocation of certification. We are considering various options to improve this framework in a more rational way. By early February, we must simultaneously announce draft amendments to the enforcement decree, enforcement rules, and public notices. We will prepare a revised innovative certification scheme that enhances predictability for pharmaceutical companies.